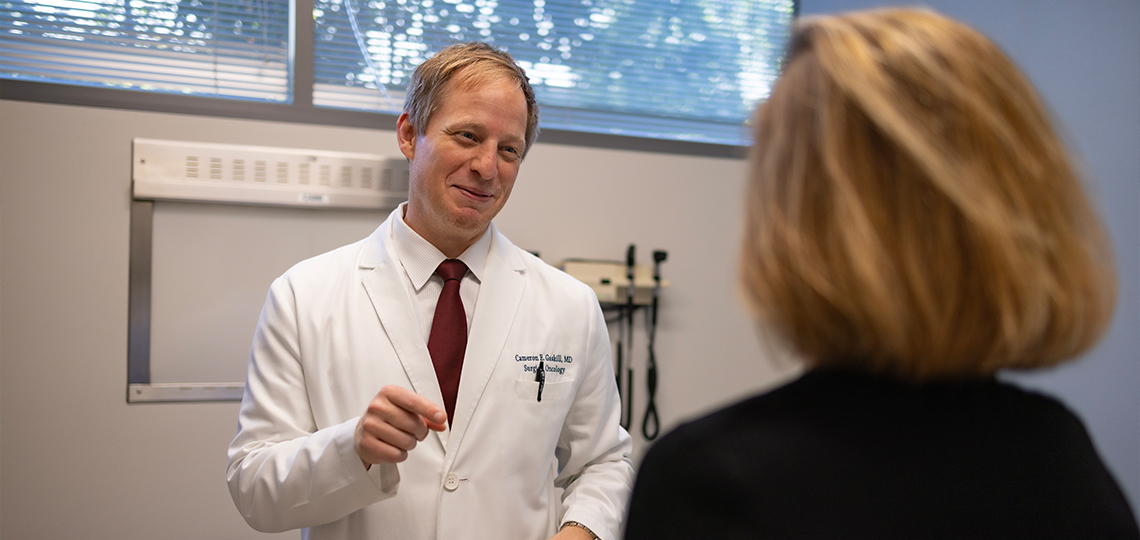
Cameron Gaskill is fellowship-trained and board-certified in complex general surgical oncology. He is the section chief for Hepato-Pancreato-Biliary Surgery and specializes in the treatment of patients with cancers of the liver, bile duct, pancreas and duodenum. He has a special clinical interest and expertise in complex surgical care, surgical innovation and robotic techniques.
What are the current trends in pancreatic cancer diagnoses and treatment?
Pancreatic cancer incidence and mortality have been slowly increasing worldwide in recent decades. It is projected to become one of the top causes of cancer death in many high-income countries. Most patients are still diagnosed at an advanced stage because early disease is often asymptomatic.
Cancer treatment is becoming more tailored to each person and uses more than one approach. Doctors are using chemotherapy before surgery more often, doing more tests to find specific gene changes, offering treatments that target those changes and working harder to catch cancer early — like using blood tests and closely watching people at higher risk.
Have you seen any shifts in the age or demographics of patients being diagnosed?
Across cancer care in general, we’re seeing important shifts in who is being diagnosed. Traditionally, most cancers were diseases of older adults, but we’re now seeing a gradual rise in colorectal, breast and pancreatic cancers among younger patients, sometimes in their 30s and 40s. The reasons aren’t fully clear but likely involve changes in lifestyle, environmental exposures and perhaps even our microbiome and metabolism.
Pancreatic cancer still remains most common in older adults, but a gradual increase in risk in younger and more diverse patient populations underscores the need for earlier recognition, better risk stratification and more equitable access to advanced care and clinical trials.
What recent advancements in treatment or early detection are most promising?
There is a lot of exciting progress being made. We are seeing significant improvements in chemotherapy combinations and in how we sequence treatments. More patients are now receiving chemotherapy before surgery, which we think helps shrink tumors, treats microscopic disease early and improves the chances of a complete resection. There’s also growing promise in personalized medicine. This means we use genetic and molecular testing to match patients with targeted therapies or clinical trials tailored to their tumor biology, and can even use the resected tumor in a vaccine to prime our immune systems to fight recurrences.
On the early-detection front, researchers are making progress in identifying blood-based biomarkers and using advanced imaging and artificial intelligence to detect pancreatic cancer earlier, especially in high-risk individuals. Here at UC Davis Health, we are part of a global clinical trial, PRECEDE, that enrolls patients with risk factors for screening with the hope that we will identify new methods of early detection and prevention of pancreatic cancer.
Why did you decide to specialize in pancreatic cancer?
I was drawn to pancreatic cancer surgery as it is one of the most challenging and meaningful areas within surgery — both technically and intellectually. Pancreatic cancer remains one of the most lethal malignancies, with limited treatment options and a devastating prognosis for many patients. Yet for some, surgery (particularly complex operations such as the Whipple procedure) offers a real chance at cure. The technical precision and meticulous judgment required in these operations are deeply compelling to me; they demand not only surgical skill but also a deep understanding of anatomy, cancer biology, physiology and multidisciplinary care.
Beyond the technical challenge, I cherish the opportunities to walk alongside patients and their families through an extraordinarily difficult journey. Caring for individuals with pancreatic cancer requires honesty, compassion, grit and persistence. It is an honor to help guide patients through decisions that often carry profound emotional weight and to be part of a team working toward hope in the face of adversity.
Specializing in pancreatic cancer allows me to combine the aspects of surgery I find most fulfilling: technical excellence, complex decision-making and deeply human connection
Aside from skiing, what are your other interests?
I love spending time with my wife and three daughters. I also sail and kiteboard. I spend significant time in Africa doing global cancer surgery work.
Cancer center joins elite group
UC Davis Comprehensive Cancer Center has been recognized as a Pancreatic Cancer Clinical Center and Academic Center of Excellence by the National Pancreas Foundation. It reflects the cancer center’s commitment to research, clinical trials, training and advanced clinical care for pancreatic cancer.