Surgery Foregut & Esophageal Motility Center
 GERD, swallowing problems, or stomach problems can be addressed via medications, endoscopic procedures (via the mouth), or minimally-invasive surgery. To properly treat your gastrointestinal (GI) problem, we have to properly diagnose GI problem and do so via different tests we offer:
GERD, swallowing problems, or stomach problems can be addressed via medications, endoscopic procedures (via the mouth), or minimally-invasive surgery. To properly treat your gastrointestinal (GI) problem, we have to properly diagnose GI problem and do so via different tests we offer:
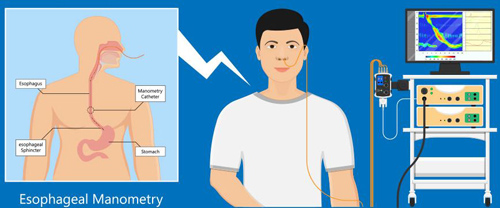
- Esophageal Manometry/Motility to assesses the movement and pressure in your esophagus.
- 24-hour pH Acid Testing to measure how much acid reflux is occurring.
- Upper Endoscopy to look inside your esophagus and stomach.
- Barium Esophagram or Upper GI X-Ray test to evaluate your anatomy.
- Esophageal Manometry/Motility Testing
 Esophageal manometry can diagnose several esophageal conditions that result in food sticking after it is swallowed. For example, achalasia is a condition in which the muscle of the lower esophageal sphincter does not relax with each swallow to allow the swallowed food into the stomach. As a result, food is trapped within the esophagus. Abnormal function of the muscle of the body of the esophagus also may result in food sticking. For instance, there may be failure to develop the wave of muscular contraction to help propel the food down the esophagus (as can occur in patients with scleroderma). The abnormal functioning of the esophageal muscle also may cause episodes of severe chest pain that can mimic heart pain (angina). Such pain may occur if the esophageal muscle goes into spasm (esophageal spasm) or contracts too strongly. In either case, esophageal manometry can identify the muscular abnormality.
Esophageal manometry can diagnose several esophageal conditions that result in food sticking after it is swallowed. For example, achalasia is a condition in which the muscle of the lower esophageal sphincter does not relax with each swallow to allow the swallowed food into the stomach. As a result, food is trapped within the esophagus. Abnormal function of the muscle of the body of the esophagus also may result in food sticking. For instance, there may be failure to develop the wave of muscular contraction to help propel the food down the esophagus (as can occur in patients with scleroderma). The abnormal functioning of the esophageal muscle also may cause episodes of severe chest pain that can mimic heart pain (angina). Such pain may occur if the esophageal muscle goes into spasm (esophageal spasm) or contracts too strongly. In either case, esophageal manometry can identify the muscular abnormality.
Esophageal manometry is also used to evaluate patients who might have gastroesophageal reflux disease (GERD). Manometry often can identify weakness in the lower esophageal sphincter – the muscle that prevents stomach acid and contents from refluxing back up into the esophagus. The procedure will also help localize the lower esophageal sphincter which would help if esophageal pH monitoring is performed.
This procedure involves passing a narrow, soft tube through the nostril and into the esophagus. This tube measures pressures so your physician can evaluate how strongly the esophagus muscles contract when you swallow and how competent the sphincter (valve) is at the end of the esophagus. In most cases it is an easily tolerated procedure. At the start of the test, you will be sitting upright. One nostril is numbed with a numbing lubricant. A thin, soft catheter is passed through your nostril, down the back of your throat, and into your esophagus and stomach as you swallow. You may feel a little pressure in your nostril and slight gagging as the tube is initially passed. This sensation subsides once the tube is in position. With the catheter in your esophagus, you will be asked to swallow small sips of water. While you are swallowing, the strength of your esophageal muscles will be measured.
Although esophageal manometry may be slightly uncomfortable, the procedure is not really painful because the nostril through which the tube is inserted is anesthetized. Once the tube is in place, patients talk and breathe normally. The side effects of esophageal manometry are minor and include mild sore throat, nosebleed, and, uncommonly, sinus problems due to irritation and blockage of the ducts leading from the sinuses and into the nose. Occasionally, during insertion, the tube may enter the larynx (voice box) and cause choking. When this happens, the problem usually is recognized immediately, and the tube is rapidly removed.
- 24 Hour pH Acid Testing
This test is used to evaluate gastroesophageal reflux. Heartburn, chest pain, and indigestion are symptoms of gastro-esophogeal reflux disease (GERD). Reflux occurs when the contents in the stomach regurgitate back up into the food pipe (esophagus). Your doctor may want to evaluate you for GERD before or after prescribing medication or performing surgery to relieve GERD. After the manometry test, that catheter will be removed. A small catheter (pH catheter) will be passed through one side of your nose. The catheter will be advanced into the esophagus and you will have a tube coming out of your nose and taped to your cheek for the next 24 hours. The catheter will remain there for the next 24 hours. The catheter will be attached to a small box Digitrapper recording device that can be secured around the waist or over the shoulder. Expect your appointment to last approximately 2 hours. The 1st study (esophageal motility study) takes approximately 45 minutes to perform. The 2nd study (24 hour pH study) takes approximately 30 minutes to perform and You will be able to drive and go to work after the procedure. You will have another appointment the next day to remove the tube and return the Digitrapper recorder.
If you are having fevers, chills, cough, upper respiratory or cold symptoms, or sinus troubles, please let us now ASAP to reschedule.
Having a sinus infection will make the testing difficult or not feasible as we will not be able to place the catheter into your nose.
NOTHING BY MOUTH 4 Hours (preferably 6) PRIOR TO THE PROCEDURE
- You may taking morning medications (such as for high blood pressure) with a small sip of water when you wake up in the morning
- If you have DIABETES, skipping breakfast may affect your need for diabetes medication; Generally you can take 1/2 of your usually dose in the morning of the test. Please review this with your primary care doctor.
- If you take a BLOOD THINNER or Plavix, please check with your Primary Care doctor that it is okay to hold this for the procedure and for how long
If it is okay to hold your blood thinner, Please hold for at least 2 days prior to the testing.
For those getting the 24 hour pH Acid Test:
7 DAYS PRIOR to testing, STOP:
Prevacid (Lansoprazole)
Prilosec (Omeprazole)
Protonix (Pantoprazole)
Aciphex (Rabeprazole)
Zegerid (Omeprazole with bicarbonate)
Nexium (Esomeprazole)
Dexilant (Dexlansoprazole)
3 DAYS PRIOR to testing, STOP:
Zantac (ranitidine)
Pepcid (famotidine)
Tagamet (cimetidine)
Carafate (sucralfate)
Bentyl (dicyclomine) - motility agent
Axid (nizatidine)
24 HOURS PRIOR to Manometry testing, STOP the following medications:
- Promotility agents (metoclopramide, bethanechol, propulsid, Reglan)
- Sedatives (diazepam, ativan, lorazepam)
- Narcotic pain medications (oxycodone, norco, morphine etc)
- Motility agents (Bentyl/dicyclomine)
If it is safe to stop these (please ask your primary care doctor), also stop these the morning of testing:
- Nitrates (I.e. nitroglycerin, nitro patches, pastes, isosorbide/Isordil, dinitrate)
- Calcium channel-blocking agents (nifedipine/Procardia, verapamil/Calan, Diltiazem/Cardizem, amlodipine/Norvasc)
- Anticholinergics (propantheline)
These medications affect the muscles of your esophagus and thus should be held 24 hours before the procedure, but may be taken immediately after the test.
MIDNIGHT PRIOR TO PROCEDURE DISCONTINUE:
Over-the-counter antacids (Maalox, Tums, Mylanta, Gaviscon)
Do NOT take a SHOWER or BATH during the study
- Try to make this a normal day by doing what you normally do.
- If you know how to bring on your GERD symptoms (certain foods, movements, activities), you are ENCOURAGED TO DO SO! There are NO diet restrictions, so you can eat what you want.
- If you stopped acid suppression medications (I.e. Prilosec/Omeprazole, Protonix/pantoprazole, Pepcid, nexium), please DO NOT restart them during this study
- Do NOT use antacids during this study, such as Tums, Rolaids, Maalox, Mylanta
- In rare instances, we do testing while patients are TAKING acid suppression meds. If this is the case, please take your medications on time and push the medication button on your Digitrapper.
- Please AVOID CONSTANT DRINKING OR SNACKING for long periods of time. You may drink beverages with meals or with snacks.
- Record every time you eat or drink in your Digitrapper (only exception is water). Eat slowly, chew thoroughly
- Do not chew gum or suck on hard candies during the study.
- You may experience increased nasal drainage during the study. You may blow your nose as usual, being careful not to snag the tube.
- Return to the Cypress Clinic the following day to have the catheter removed. Do not forget to bring your 24 hour diary with you.
- Once you are done with the 24 hour pH acid test, you may resume all acid suppression drugs
DIARY and DIGTRAPPER Instructions
- RECEIVER goes into SLEEP MODE after 30 sections. WHEN RECEIVER IS IN SLEEP MODE, you will need to press your SYMPTOM BUTTON (COUGH, HEARTBURN, REGURG), MEAL, or LYING DOWN BUTTON TWICE TO ACTIVATE.
- USE THE TIME DISPLAYED ON THE RECORDER, WHEN MAKING ENTRIES INTO THE DIARY.
- RECORD YOUR MEALTIME FROM BEGINNING TO END, AS WELL AS SYMPTOMS.
- RECORD WHAT TIME YOU BEGIN TO LAY DOWN AND WHAT TIME YOU GOT UP.
Bring your diary in with you when you return the next day to have the monitor removed.
If you have any questions, please call the Bariatric/Cypress Surgery Clinic at 916-734-2680 Mon-Fri between 8 a.m. - 4:30 p.m. for assistance. After hours, call 916-734-2011 and ask for the Bariatric Surgery Team to be paged.
 - Upper Endoscopy | Esophagogastroduodenoscopy (EGD)
- Upper Endoscopy | Esophagogastroduodenoscopy (EGD)
During this procedure, after receiving sedating medications by anesthesiologists, your surgeon will use a flexible tube called an endoscope, which contains a light and video camera, to look at the inside of your esophagus, stomach, and duodenum (first part of the small intestine).
This is helpful to look for inflammation in the esophagus or stomach, polyps, ulcers, and a hiatal hernia, which may be causing your symptoms. A biopsy of tissue may be performed to look at the tissue under a microscope to diagnose certain diseases. This does not hurt.
Your Endoscopy will be performed at:
UC Davis University Tower GI Lab
2315 Stockton Blvd.
Sacramento, CA 95817
University Tower, 2nd Floor
Please call 916-734-2890 to schedule it. If you have trouble reaching someone at the number, try 916-734-5918 or 916-734-4575.
You will have to perform at at-home COVID test 1-3 days before your procedure. If it is positive, please let the GI lab know. If the testing is not completed within the time frame or has positive results, then the procedure will be cancelled.

If you have any issues or need to cancel, please call at least 3 days in advance.
DRIVER: You must have a responsible adult family or friend who can drive you home. NO bus, taxi, Lyft, Uber allowed unless you are with an adult friend or family member. No driving the remainder of the day.
Please reach out to your prescribing physician if you're taking the following medication(s) 7 days prior to your procedure:
- Blood Thinners: If you are taking blood thinners such as: clopidogrel bisulfate (e.g. Plavix®), warfarin (e.g. Coumadin®, Jantoven®), rivaroxaban (e.g.Xarelto®), apixaban (e.g.Eliquis®), ticagrelor (e.g. Brilinta®), dabigatran (e.g.Pradaxa®), heparin, or aspirin (325 mg) contact the prescribing physician right away for instructions.
- Diabetes: If you have diabetes and are using insulin or are taking oral diabetes medications, contact your primary care doctor for instructions on adjusting these medications for the day of your procedure.
5 Days Before Procedure:
- Avoid ibuprofen (e.g. Motrin®, Advil®), naproxen (e.g. Aleve®, Naprosyn®), celecoxib (e.g. Celebrex®), rofecoxib (e.g.Vioxx®), or medications containing aspirin 5 days prior to procedure.
- Okay to take aspirin (81 mg).
- You may take acetaminophen (e.g. Tylenol®) if needed.
Do not eat anything 8 hours before your arrival time.
Do not drink anything 3 hours before your arrival time.
Day of Procedure:
- You may only have clear liquids up until 3 hours before your procedure.
- Clear liquids include: Water, Clear juices (apple or white grape), Flavored water, Popsicles without fruit or cream, Jell-O, Gatorade, sodas, Black coffee or tea without creamer.
-
- NO red, purple, or blue dye
- NO broth after midnight, the night before your procedure.
- NO milk/dairy products
- NO alcohol
- NO solid foods
- NO orange juice and cranberry juice
- If you take medication for blood pressure, heart, seizure, or pain, please take these with just a sip of water at least 3 hours before your appointment.
- Remove all jewelry and body piercings before your arrival. If you use a C-PAP machine, inhaler, or Bi-Pap, please bring these with you.
- Barium Esophagram and Upper GI X-Ray Series
- This test is an X-ray that takes pictures of the esophagus, stomach, duodenum and small intestine.
- You will need to drink a chalky liquid called barium while X-ray pictures are taken. The barium makes it easier for the health care provider to see.
- These pictures can be used to make a diagnosis and plan more specific treatments.
- This is done by radiology and you should call 916-734-0655 to schedule the test.
- The ENT clinic also offers this and you can call 916-734-5400 to schedule the test.





