Vasectomy Reversal
A vasectomy reversal is a surgical procedure where the vas deferens is reconnected after a patient has had a vasectomy. This procedure is done for each vas deferens, of which there are two. The goal of a vasectomy reversal is to restore sperm to a man’s semen, allowing the possibility of natural conception after a previous vasectomy. Although rare, it’s also used to relieve pain associated with congestion that may occur from a vasectomy.
Frequently Asked Questions (FAQs)
Operating time for a vasovasostomy or epididymovasostomy is approximately 3 hours. A general anesthetic is preferred in most circumstances. We prefer that out-of-town patients stay in the Sacramento area for at least one day after surgery.
Postoperative follow-up includes an evaluation of wound healing at 2-3 weeks and a semen analysis at 6-8 weeks after surgery. Insurance will typically not cover this semen analysis fee. Subsequent semen analyses may be needed to monitor the return of sperm.
Vasectomy reversal fees vary depending on insurance coverage, so please contact us for more information. Sperm banking at the time of surgery is also available (see below). A 2-week postoperative wound evaluation is included in the surgical fee. Charges for the hospital and anesthesia are billed separately from the surgeon’s fee.
At the time of the procedure, you have the option to harvest sperm to freeze for future use. Contact our office for current pricing.
Any additional office visits and semen analyses, including postoperative semen analysis, will be charged at the usual rates. Also, if you choose to have sperm cryopreserved, you may incur costs of infectious disease testing required by the U.S. Food and Drug Administration (FDA).

The area where the vasectomy was done is identified and the tissues around are dissected off.
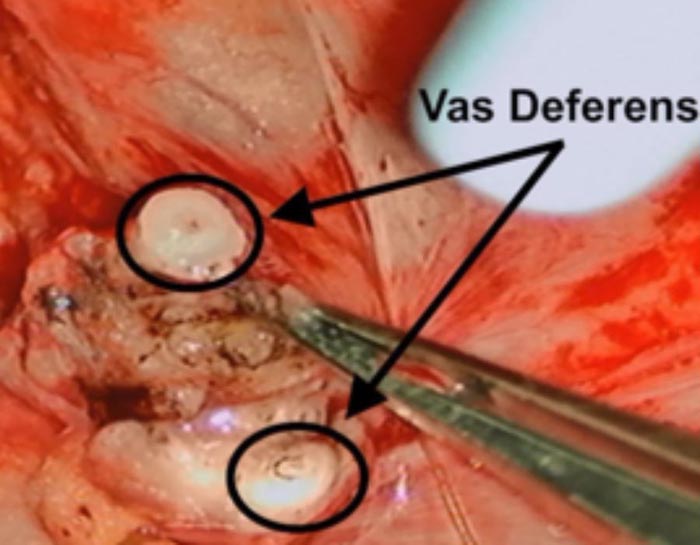
The vas deferens is then cut above and below the vasectomy site exposing healthy, unscarred vas deferens. The top side goes to the abdomen and the bottom side to the testicle.
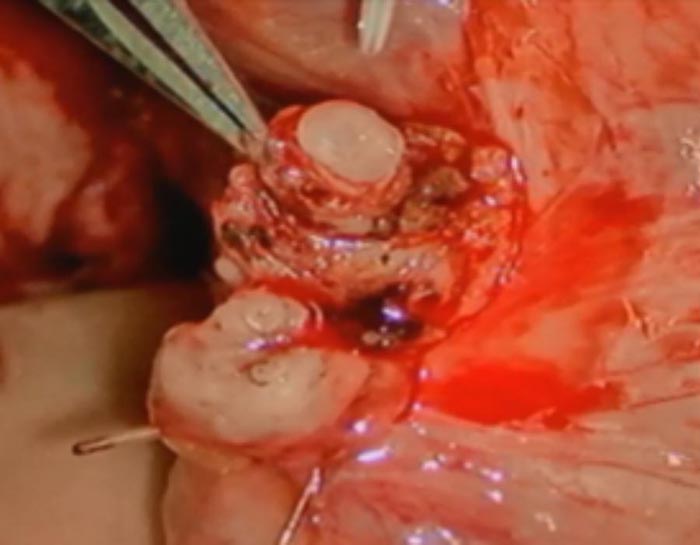
The fluid from the bottom side (testicular side) of the cut vas deferens is tested for quality and sperm content. This determines whether the surgeon reconstructs using a vasovasostomy or vasoepididymostomy approach (see figures above).
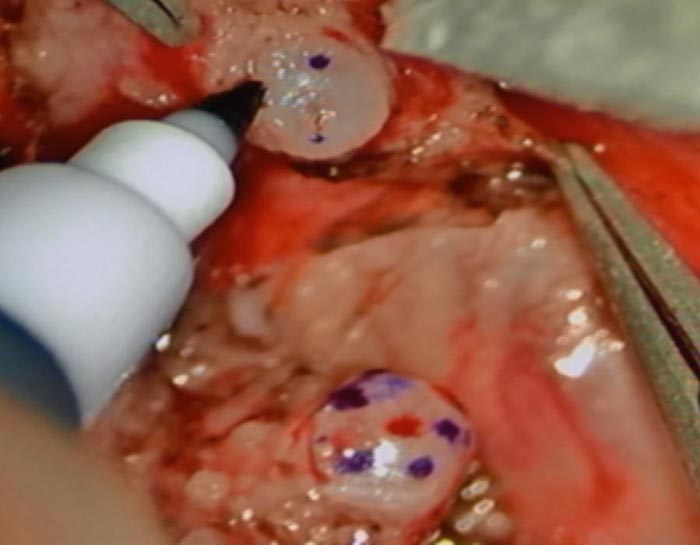
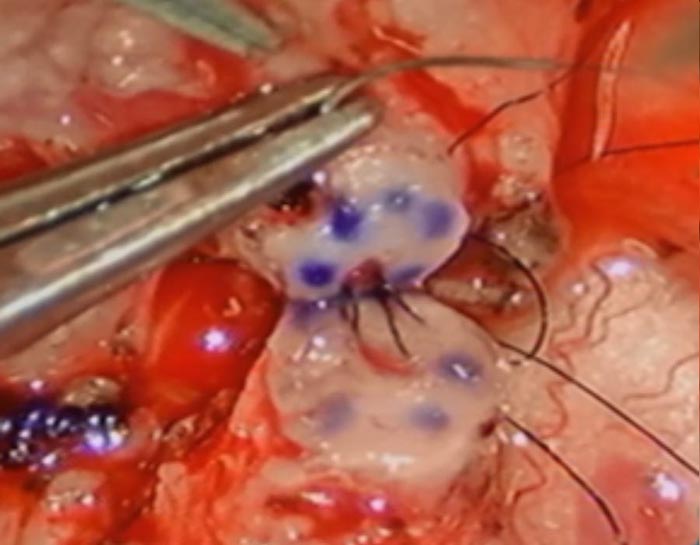
This patient required a vasovasostomy. The sites where we placed sutures are marked prior to starting the reconnection.
This photo shows the use of a single layer (9-0 nylon) to approximate the vas deferens cut ends. Our team often uses a 3-layer closure using 10-0 nylon to bring the lumens of the tubes together more precisely.
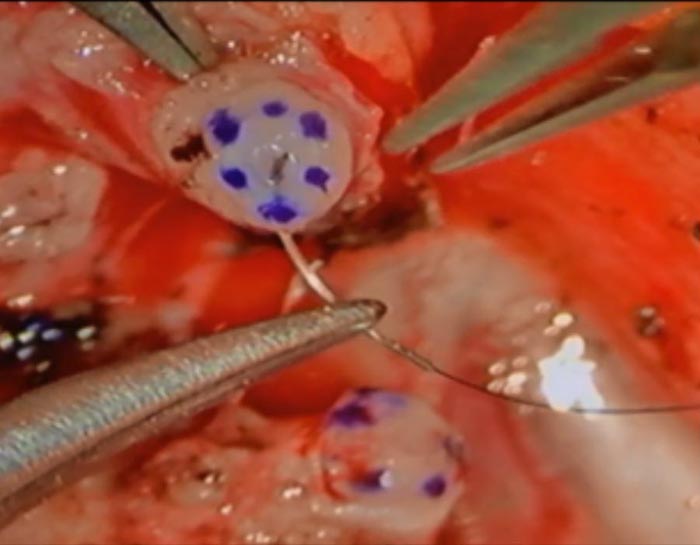
The sutures are carefully tied to bring the lumens of the tubes together.
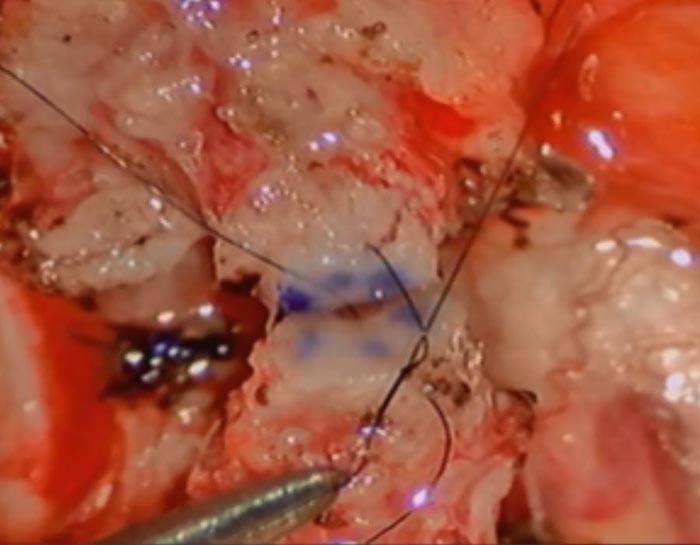
Care is taken to keep the knots out of the lumen.
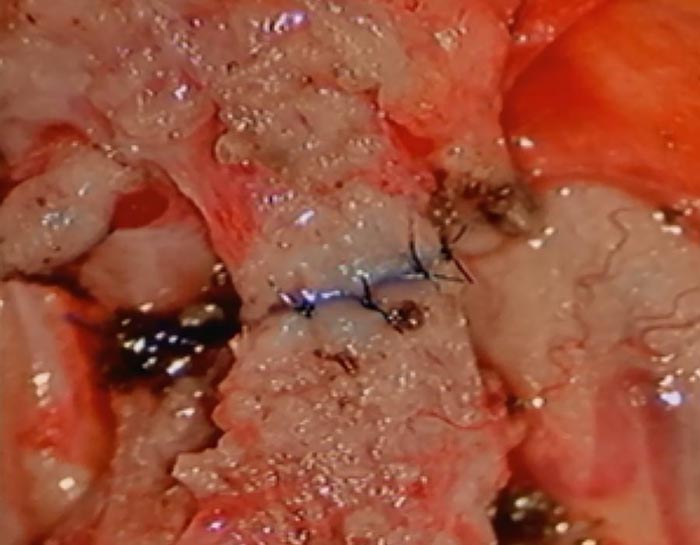
The final result is shown here, a re-approximation of the vas deferens in this case.
The success of a vasectomy reversal depends on a combination of the skill of the surgeon and the findings at the time of surgery.
When the vas is opened, fluid will flow from the testicular side of the vasectomy site. If sperm are present, a vasovasostomy will be performed (see figure). We expect about 95% or more of these patients to demonstrate a return of sperm to the ejaculate, with an associated 60-70% pregnancy rate. If no sperm are present, but the vasectomy fluid appears to be abundant and ultimately suitable for sperm production (e.g., clear, watery), then a direct vasovasostomy is performed, with the expectation of a successful outcome such as that described above.
If poor-quality fluid is present (e.g., thick or pasty) and sperm are absent, or no fluid at all is found, then an vasoepididymostomy (connection of the vas to the epididymis, see figure) is performed, with return of sperm to the ejaculate in 65% of our patients.
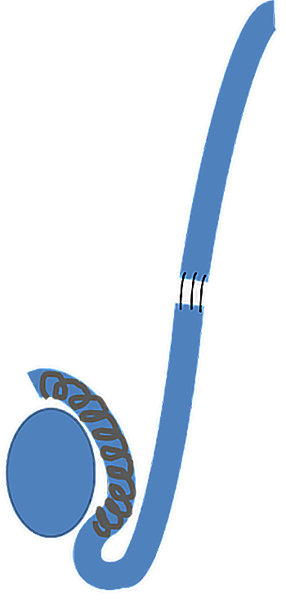
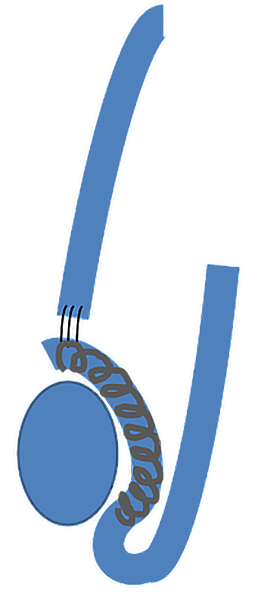
Image Description
(Left) Vasovasostomy: Connecting vas deferens to vas deferens
(Right) Vasoepididymostomy: Connecting vas deferens to tubules in epididymis
