October 2020 - Presented by Miao Tian (Mentored by Denis Dwyre)
Clinical History
A 65-year-old female with splenomegaly, hepatomegaly, and adenopathy presents for a lymph node biopsy to rule out lymphoma. She has leukopenia with a white count of 3,700 and thrombocytopenia with a platelet count of approximately 100,000, which has been present since at least February 2018. Her bilirubin is elevated at 1.7 mg/dL. Liver function tests are normal and her CBC red cell indices (MCV, MCH, and MCHC) are also normal. Hepatitis B and C testing was negative. LDH is normal at 188 U/L. Molecular testing for JAK, CALR, and MPL are negative. An abdominal and pelvic CT with contrast found splenomegaly at 18.2 cm and hepatomegaly at 18.5 cm.
Pathology Review
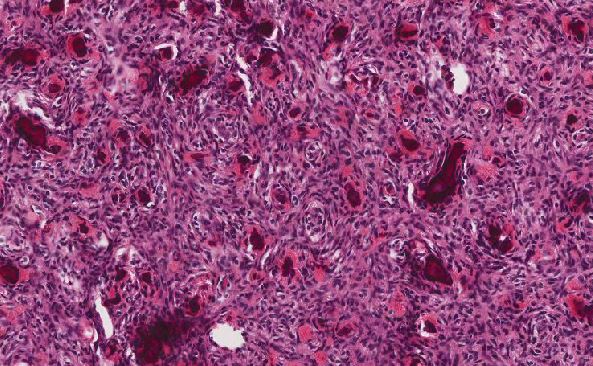
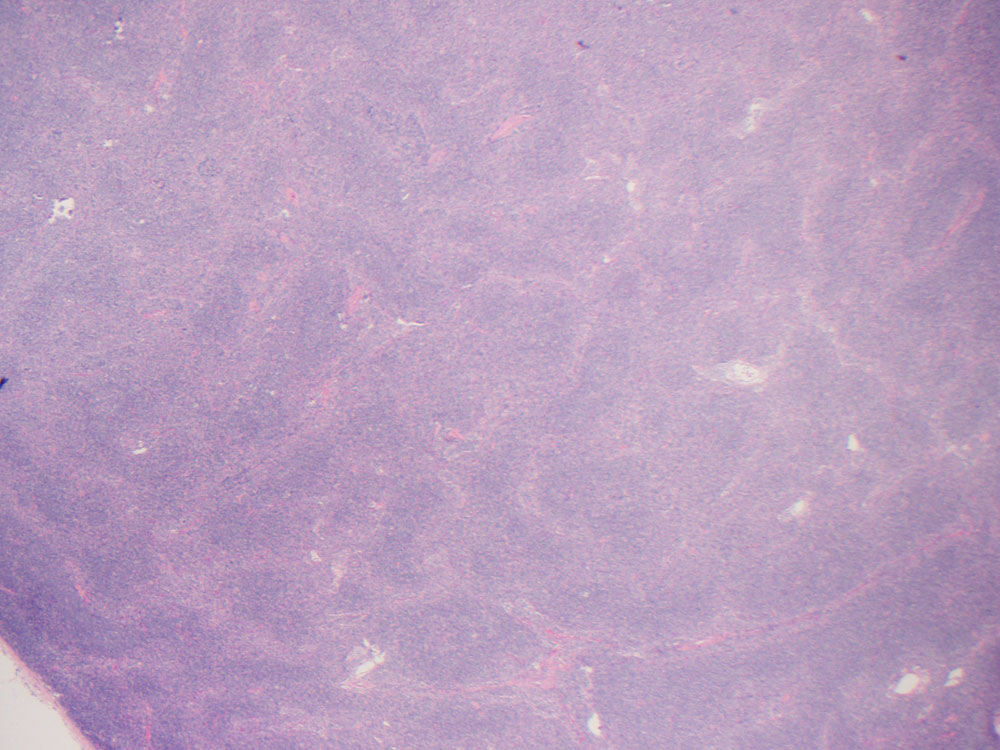
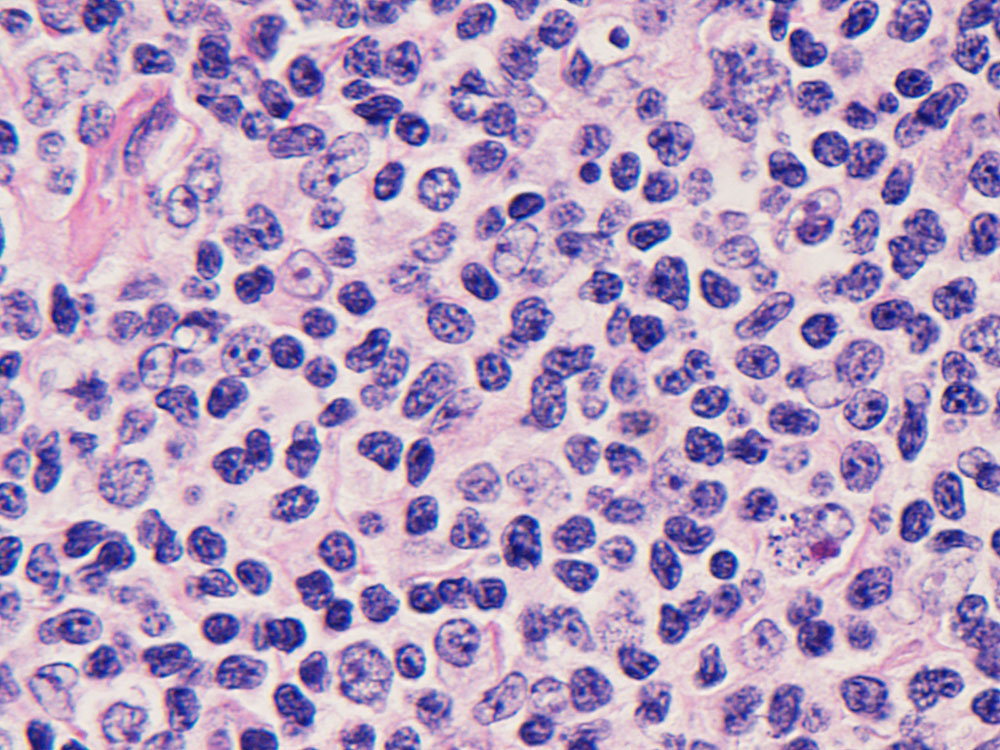
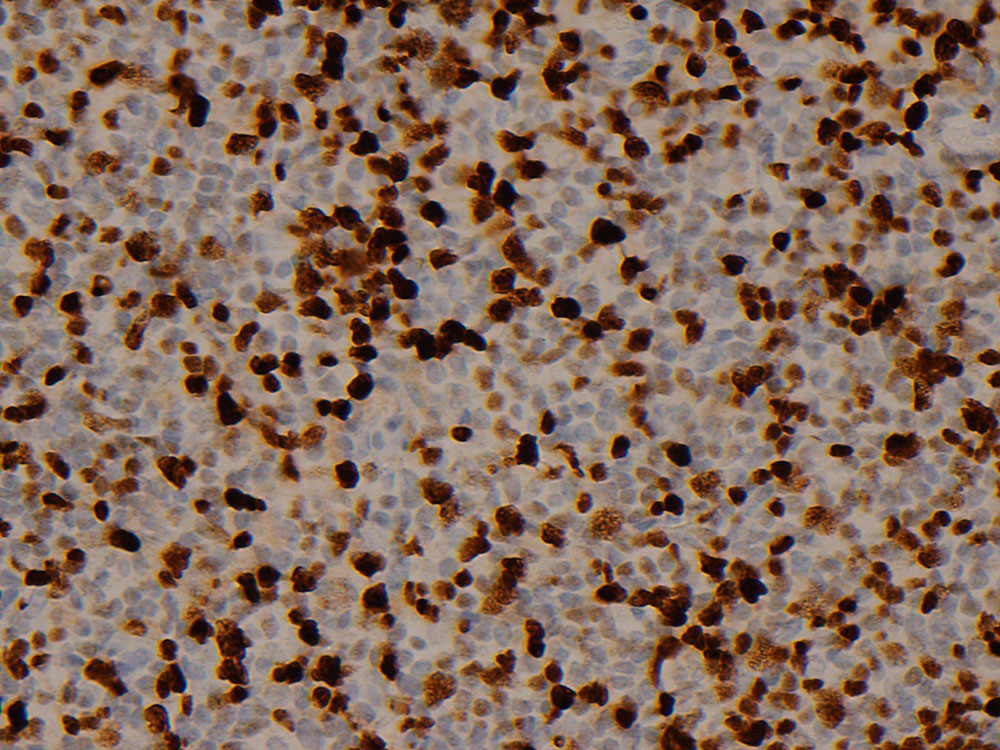
Biopsy from a left groin lymph node reveals an effaced nodal architecture with an atypical lymphoid proliferation (Figure 1) which is composed of small to medium sized monocytoid cells with slightly irregular nuclei, coarse chromatin, inconspicuous nucleoli and moderate amount of pale cytoplasm. Scattered large atypical cells are also noted (Figure 2).
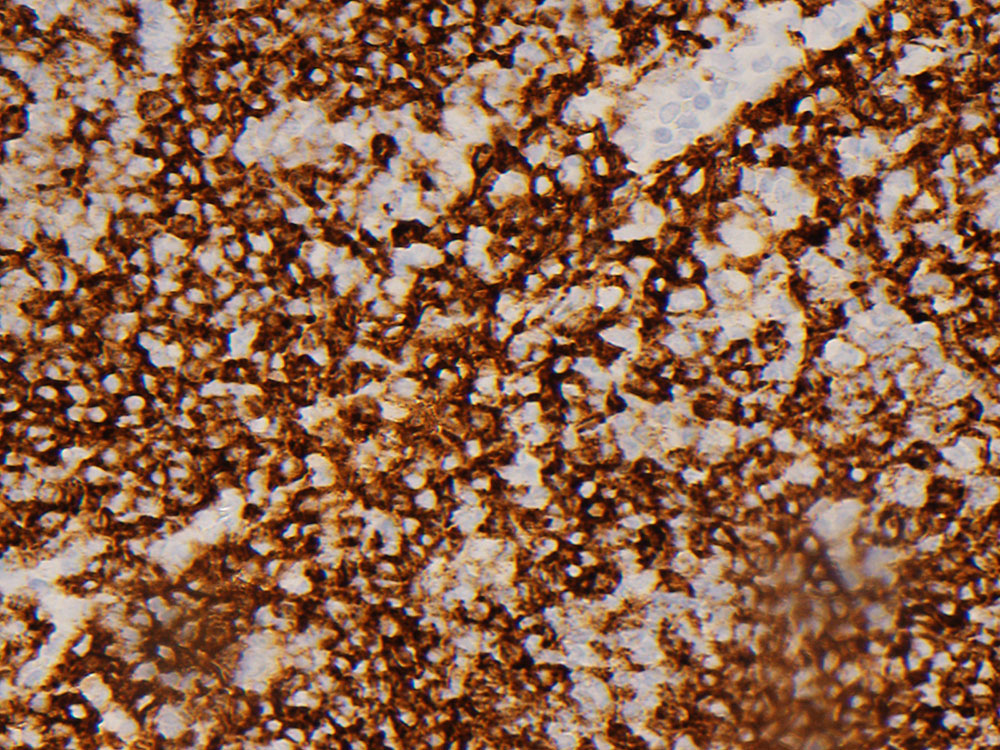
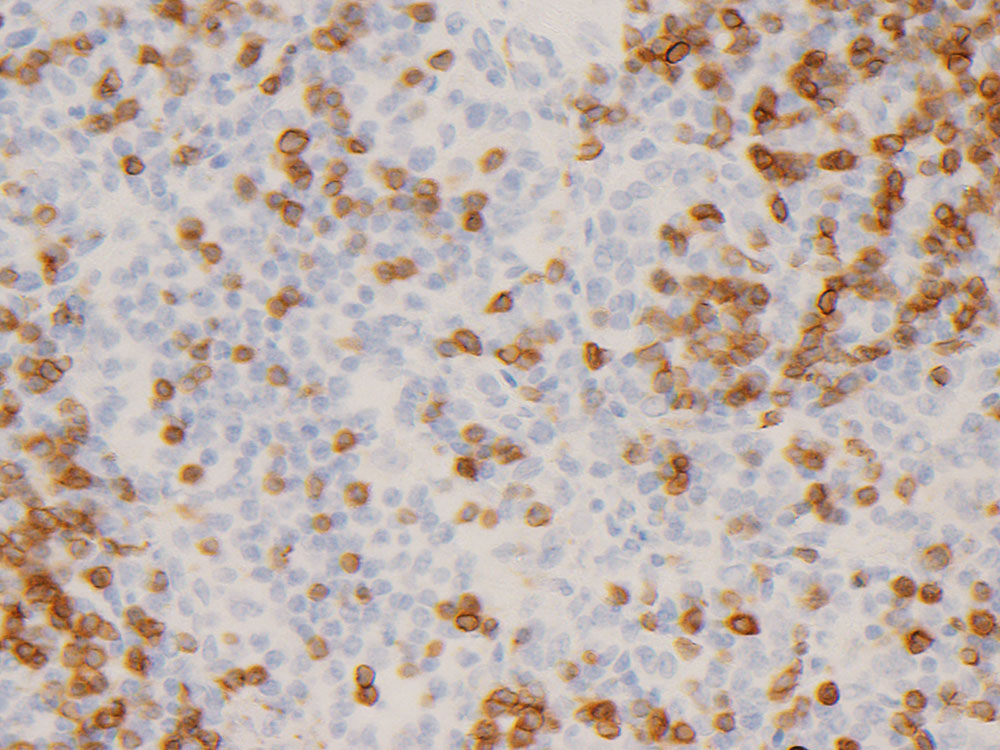
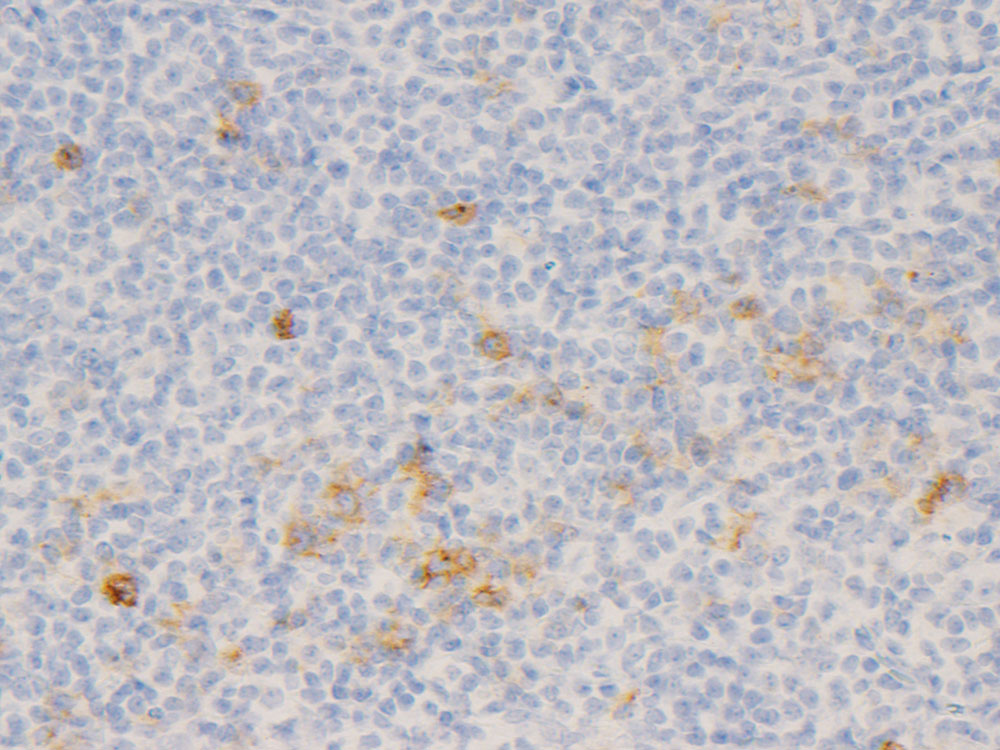
Immunohistochemical stains show that the monocytoid cells are positive for CD20 (Figure 3), PAX5, CD79a and OCT2 (Figure 4), and negative for CD3, CD5 (Figure 5), CD10, CD30 (Figure 6) and BCL1.

 Meet our Residency Program Director
Meet our Residency Program Director