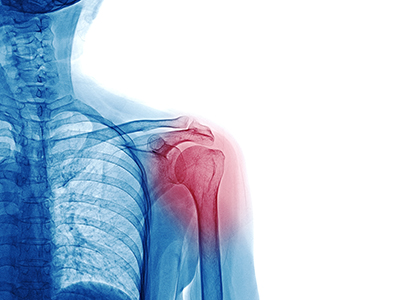
It’s shoulder arthritis – now what?
Shoulder arthritis can be addressed in a variety ways depending on your goals, from conservative treatment to the latest surgical techniques.
 So you think (or know) that it’s shoulder arthritis or shoulder bone spurs. The joint hurts during your favorite activities and in your work around the house. Sometimes it hurts at night.
So you think (or know) that it’s shoulder arthritis or shoulder bone spurs. The joint hurts during your favorite activities and in your work around the house. Sometimes it hurts at night.
Is this going to be par for the course from now on?
First of all, know you’re not alone. Shoulder arthritis leads to upper body dysfunction in over 20 million Americans, or about 6% of us. At UC Davis in Sacramento we see (and treat) arthritis in the shoulder from a wide variety of causes, ranging from traumatic injury and wear and tear, to diseases such as rheumatoid arthritis or sickle cell disease.
Also, know that you don’t have to live with shoulder arthritis symptoms if you don’t want to. There are options, and new insights and refinements emerge every year. A knowledgeable surgeon, who monitors the latest developments in the field, can help you gauge the pros and cons of different existing and emerging treatment paths, in relation to your goals and your risk tolerance.
As is the case in all areas of medicine, the body of knowledge about shoulder arthritis and treatments is growing all the time.
Shoulder arthritis symptoms and diagnosis
About the author
Dr. Bayne is chief of hand, shoulder and upper extremity surgery at UC Davis Health in Sacramento, specializing in conditions involving the shoulder, hand and elbow.
He attended some of the nation’s most prestigious medical schools and orthopaedic training programs.
- M.D., Harvard Medical School
- Internship and Residency, Rush University Medical Center
- Fellowship, Mayo Clinic
First of all, an accurate diagnosis is important for shoulder arthritis. The shoulder is an incredibly complex interplay of multiple bones, joints, muscles and nerves. It handles lots of forces and torque.
Pain, weakness and mobility issues can be linked to a variety of primary or secondary injuries. These can range from problems with the muscles that make up the rotator cuff, to tendonitis, to impingement of nerves and tendons caused by inflammation or actual structural changes. You also want to be sure to rule out nerve issues or damage.
There are two main joints in the shoulder that become arthritic, each with different responsibilities, paths to damage, and treatments:
- The joint in the top of the shoulder is the more likely place to experience arthritis. Known as the acromioclavicular joint – or the friendlier “AC joint” for short – it’s the place where your collarbone (the clavicle) meets the shoulder blade (the acromion).
- The ball-and-socket joint on the outside of the shoulder is known as the glenohumeral joint or the GH. It is made up of the humerus (ball) and glenoid (socket).
Treatment options for shoulder arthritis
Improvements in surgical implants and technique have significantly increased patient pain relief, function, and longevity of positive results.
Most patients with AC joint arthritis can be treated nonoperatively with rest, activity modification, and therapy. Corticosteroid injections may sometimes provide relief.
For those who have symptoms that do not improve with conservative treatment, a surgical distal clavicle resection may be indicated. Your surgeon will remove the arthritic part of the collarbone, and scar tissue will take its place to allow you to continue moving your shoulder joint with less pain.
Shoulder replacement, or minimally invasive repair?
As with AC arthritis, the first line of treatment for GH arthritis is nonoperative. If this does not improve symptoms, surgery may be indicated. Shoulder replacement is the treatment of choice for patients over the age of 55 with significant GH arthritis.
What to do with younger patients can sometimes be less clear-cut, and is a matter of discussion and ongoing research in the field. They generally need to return to heavier use of the joint, and need the results of surgery to last much longer.
 Some small studies report good initial results for shoulder replacement in younger patients – such as return to activity at seven months with high patient-satisfaction levels, according to research covered by the American Academy of Orthpaedic Surgeons. However, there are time and scope limitations on that data.
Some small studies report good initial results for shoulder replacement in younger patients – such as return to activity at seven months with high patient-satisfaction levels, according to research covered by the American Academy of Orthpaedic Surgeons. However, there are time and scope limitations on that data.
Non-shoulder replacement options in the younger patient can include arthroscopic "key hole" debridement, partial joint replacement, and joint resurfacing, in which biologic tissue is used to line the joint.
It can come down to a matter of assessing balance — the patient’s goals for returning to work, sports or other activity in the short term, versus the long-term risk of needing follow-up or “revision” surgeries to replace a worn-out implant, or tighten one that’s loosened over time. Whether a procedure will create a “point of no return” that limits future surgery options is also a consideration.
A surgeon who's familiar with both the overall and emerging literature can help interpret options for your goals.
What kind of shoulder replacement?
Shoulder arthritis: More information
Shoulder replacement is a surgery in which the patient's natural bone in the ball-and-socket joint of the shoulder is replaced with synthetic material, most often metal or plastic. Shoulder replacement typically falls into one of three categories:
Anatomic total shoulder replacement: The ball on the top of the humerus is replaced with a metal ball. The socket gets covered with a new plastic surface. Anatomic shoulder replacements are performed for patients with GH arthritis that have plenty of strong, normal bone.
Partial shoulder replacement: Only the ball on the top of the humerus is replaced. Partial shoulder replacements are significantly less commonly performed. They may be an option for younger patients, and patients with problems of the humerus alone. They are sometimes performed in patients with shoulder arthritis that also have problems with the nerves that supply the deltoid (shoulder) muscle.
Reverse shoulder replacement: The socket is implanted on top of the humerus, and the ball is implanted on the native bony socket. Reverse total shoulder replacements are performed for patients with GH arthritis who also have problems of the rotator cuff. They may also be performed for patients with glenoid (socket) bone loss or patients with severe humerus fractures.
Shoulder replacement implants may have several variations in design, including differences in shape, size and construct. Examples include short-stemmed, long-stemmed, and stemless humeral head replacements, or a design that allows the ability to add bone graft when necessary. These options help the experienced surgeon tailor the procedure to the specific needs, anatomy, and physiology of the individual patient.
The outlook for shoulder arthritis
Appointment requests
Dr. Bayne and his hand, shoulder and upper extremity surgery team are part of the nationally ranked UC Davis Health Department of Orthopaedic Surgery.
Shoulder arthritis can be debilitating. Fortunately, we have nonsurgical and surgical treatment options that can relieve pain and help patients regain a happy, healthy lifestyle. Improvements in surgical implants and techniques have significantly increased patient pain relief, function, and longevity of positive results.
At UC Davis Medical Center in Sacramento, our surgeons combine expertise and experience in the treatment of shoulder arthritis. In addition to treating patients with common presentations, we also have significant experience treating patients with less common or more severe presentations of shoulder arthritis, including patients with inflammatory arthritis, post-traumatic arthritis, and arthritis with nerve injury or partial paralysis.
Your doctor is your gateway to the constant, and often amazing, advances in understanding and treatment options across the field of orthopaedic surgery. To achieve your maximum benefit, look for someone who will listen to your concerns and goals – and then be fully equipped to help explain and interpret the latest pathways, and the pros and cons as they relate to you.

