Resident Program - Case of the Month
December 2018 - Presented by Tahera Iqbal (Mentored by Regina Gandour-Edwards)
Discussion
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma (ACC) is a rare type of tumor that accounts of approximately 10% of all salivary gland tumors. It is the most common malignant tumor of the submandibular and minor salivary glands. Grossly, the tumor is solid and can have infiltrative pattern of growth although some examples can be well circumscribed. The infiltrative capacity is a hallmark of this salivary gland carcinoma. They can spread along the nerve sheaths and can cause tenderness, severe pain and or even facial nerve paralysis. They can also infiltrate into fat, skeletal muscle, soft tissue destroying the residual salivary gland tissue. Microscopically, however, it extends beyond the visible and palpable lesion. It is a malignant epithelial tumor with epithelial and myoepithelial cells arranged in a tubular, cribriform or solid form.
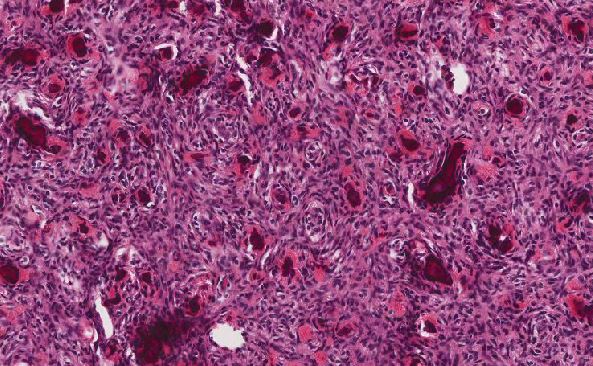
Combination of pattern may be present in the tumor; however, one usually predominates. The three types of patterns typically encountered are cribriform, tubular and solid. The cribriform pattern consists of concentrically arranged epithelial cells around pseudocysts filled with amorphous glycosaminoglycans and/or hyalinized basal lamina. The extracellular spaces are not true glandular lumina but rather are part of the tumor stroma. Majority of the ACC is predominated by the cribriform pattern. The tubular pattern consists of lumen that are more conspicuous, with true lumina surrounded by smaller ductlike arrays of basaloid epithelial cells. Higher magnification shows cells surrounding the spaces are haphazardly oriented, with the small nests separated by hyalizined stroma. The solid pattern is the least frequently encountered and it is most often mixed with another variant of ACC. It is characterized by solid nests of basaloid cells often in a hyalinized stroma. It can display a greater degree of pleomorphism than the other variants, and mitotic rate may be slightly increased. However, alternate diagnosis should be considered if marked pleomorphism, high mitotic rare and enlarged nuclei with prominent nucleoli is encountered.
Differential Diagnosis
Polymorphous low-grade carcinoma (PLGA) is in the top differential when it comes to considering adenoid cystic carcinoma especially the tubular variant. PLGA is an indolent neoplasm that is often identified in the minor salivary glands and is the most common glandular malignancy in the palate. It is characterized by cells that display single cell invasion, often in columns or rows with seen with perineural invasion. Close examination shows plump columnar cells with more prominent eosinophilic cytoplasm than the distinctly basaloid cells of ACC. Immunohistochemical results show that CD117 and S-100 are the best markers to distinguish PGLA from ACC. Staining for CD117 is stronger and more diffuse inn ACC when compared to PGLA while S-100 shows the reverse.
Pleomorphic adenoma also known as benign mixed tumor is a benign epithelial tumor that shows epithelial, myoepithelial and mesenchymal differentiation. It is the most common neoplasm of the salivary gland and typically present as painless persistent swelling that can occur at any age. Approximately, 75% of the tumor arise in the parotid gland with the remaining occurring in the submandibular gland and minor salivary gland. Microscopically, the epithelial component may have solid, tubular, trabecular or cystic architectural pattern. The stroma can be quite variable which may include myxoid, mucoid, fibroblastic, cartilaginous, osseous and lipogenic component.
Basal cell adenoma is a rare epithelial neoplasm that displays monomorphic basaloid cells without a myxochondroid component representing 1%-3% of all salivary gland neoplasm. Approximately, 70% of this tumor arise in the parotid gland with the remaining occurring in submandibular gland and other sites in the oral cavity. Grossly, these are well demarcated, encapsulated masses with the cut surface that can display solid, homogenous or cystic features. Apart from the membranous subtype, the presence of a capsule is an important distinguishing factor when comparing to ACC. The basement membrane separates the tumor cells from the nonmucoid stroma. Histologic pattern includes solid, trabecular, membranous or tubular growth of epithelial cells resembling pleomorphic adenoma but with peripheral palisading. The lack of infiltrative growth and perineural invasion also distinguishes this tumor from ACC.
Basal cell adenocarcinoma is a rare low-grade malignant counterpart of basal cell adenoma. The most common location of this lesion is the parotid gland. It shows myoepithelial differentiation identical to basal cell adenoma, but differs by having infiltrative growth pattern, perineural spread, vascular invasion and a capacity for metastasis. It accounts for 1-2% of salivary gland carcinoma with 23% arising within pre-existing basal cell adenoma. A portion of the tumor may be partially encapsulated but has at least have focal invasion into the adjacent salivary gland. Most basal cell neoplasm has β-catenin expression; therefore, β- catenin immunostaining may aid in the differential diagnosis between basal cell neoplasm and ACC.
References
Brookstone M, Huvos AG, Spiro RH. Central adenoid cystic carcinoma of the mandible. J Oral Malxillofac Surg 1990; 48:1329-1333
Perzin KH, Gullanee P, Clairmont AC. Adenoid cystic carcinoma arising in salivary glands. A correlation of histologic features and clinical course. Cancer 1978; 42: 265-282
Sternberg, Stephen S., Stacey E Mills, and Darryl Carter. Sternberg's Diagnostic Surgical Pathology. 6th ed. Philadelphia: pp (906-942) Wolters Kluwer Health/Lippincott Williams & Wilkins, 2010.
Zhan KY et al: Basal cell adenocarcinoma of the major salivary glands: A population-level study of 509 cases. Laryngoscope. 126(5):1086-90, 2016
Li BB et al: Basal cell adenoma of salivary glands with a focal cribriform pattern: clinicopathologic and immunohistochemical study of 19 cases of a potential pitfall for diagnosis. Ann Diagn Pathol. 18(1):5-9, 2014
Anderson C, Krutchkoff D, Pederson C, et al. Polymorphous low-grade adenocarcinoma of minor salivary gland; a clinicopathologic and comparative immunohistochemical study. Mod Pathol 1990; 3: 76-82
Rooper L et al: Polymorphous low-grade adenocarcinoma has a consistent p63+/p40- immunophenotype that helps distinguish it from adenoid cystic carcinoma and cellular pleomorphic adenoma. Head Neck Pathol. 9(1):79-84, 2015
Triantafyllou A et al: Functional histology of salivary gland pleomorphic adenoma: an appraisal. Head Neck Pathol. 9(3):387-404, 2015
Thompson, Lester D., Wenig, Bruce M. Diagnostic Pathology: Head and Neck, 2nd edition. Philadelphia pp (517-520) Elsevier, 2017

 Meet our Residency Program Director
Meet our Residency Program Director