Resident Program - Case of the Month
Novermber 2017 - Presented by Ying Liu (Mentored by Alaa Afify)
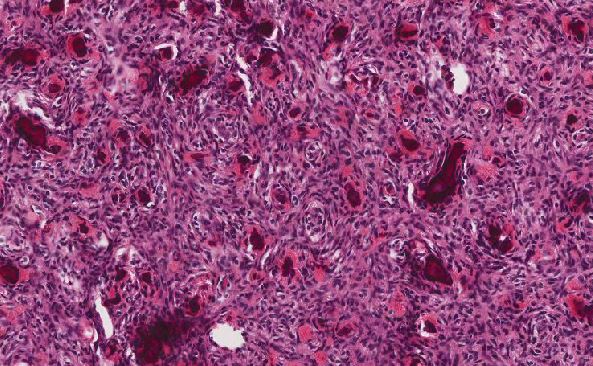
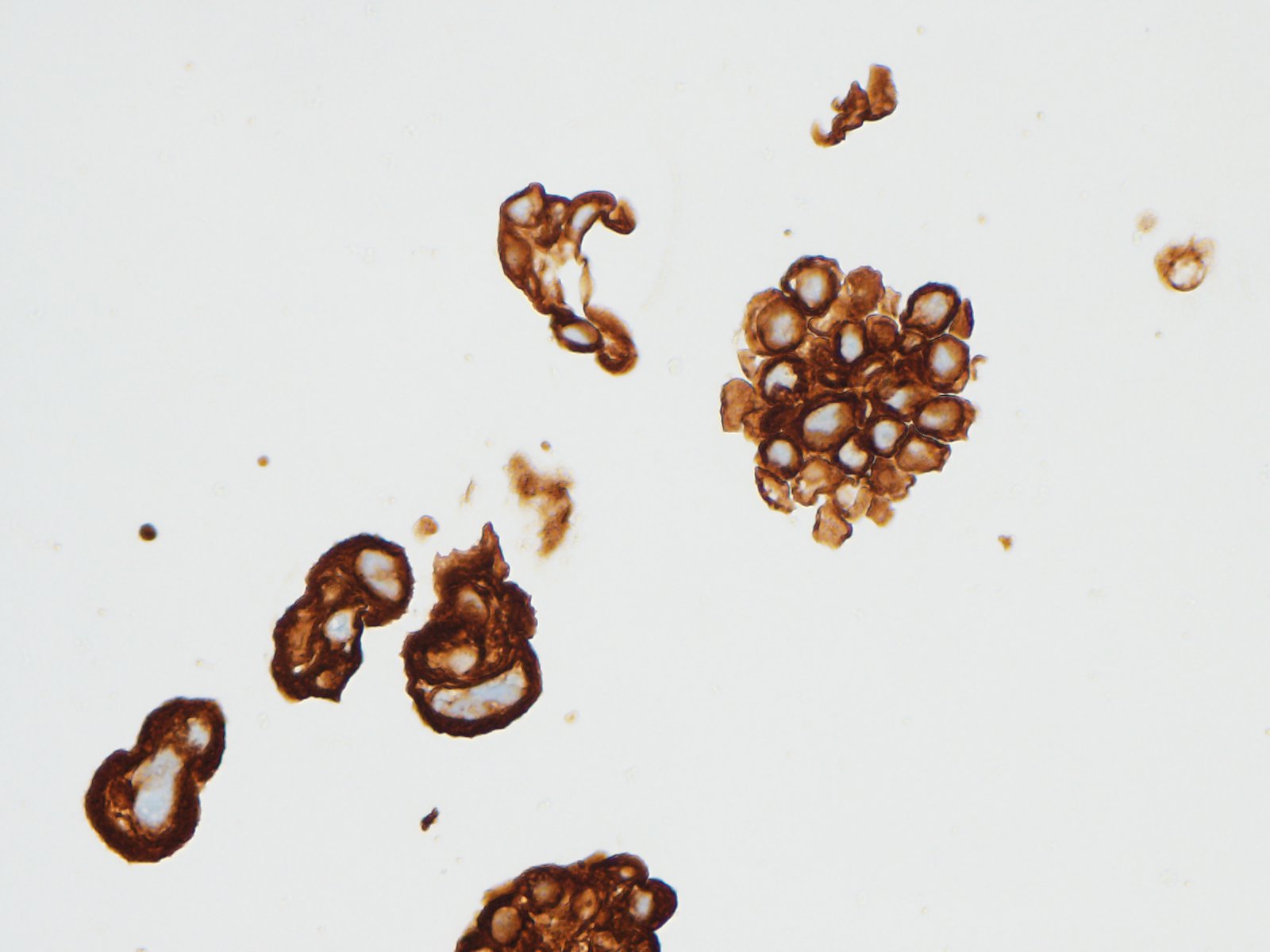
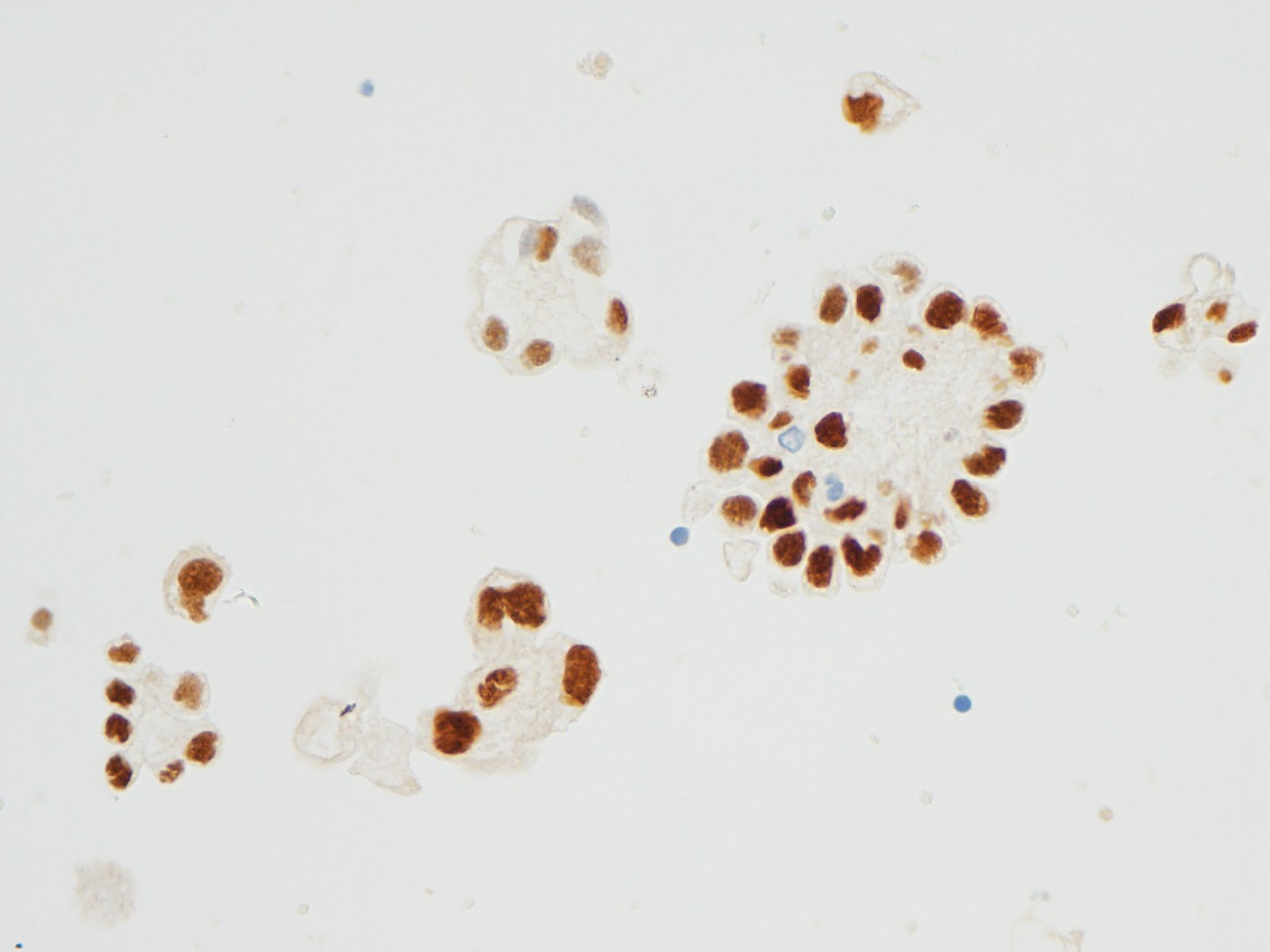
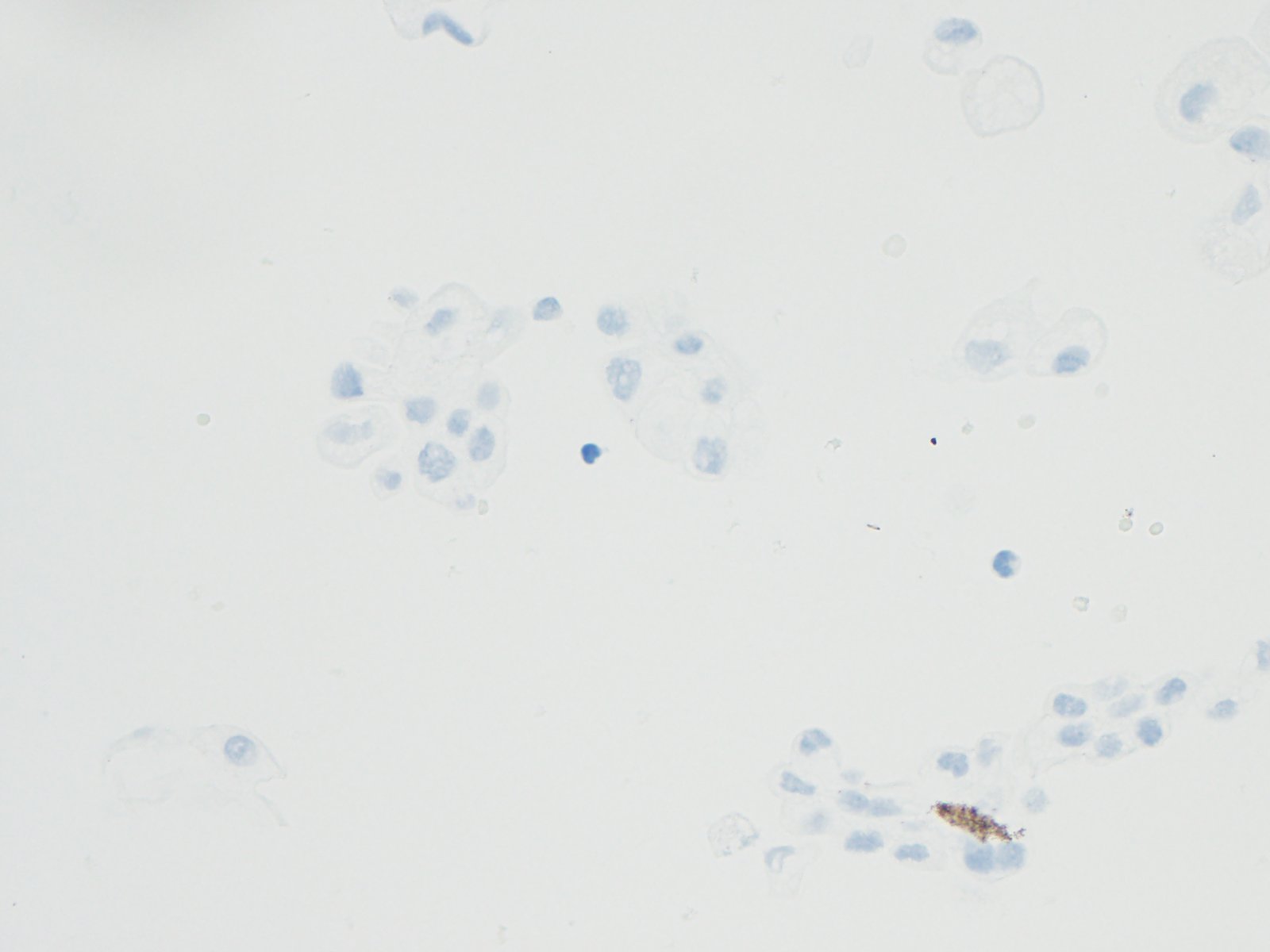
Immunohistochemistry stain in neoplastic cells are showed in Figures 5-8
Click on image to enlarge.
| Figure 5: >CK7 40x | Figure 6: CK20 40x | |
 |
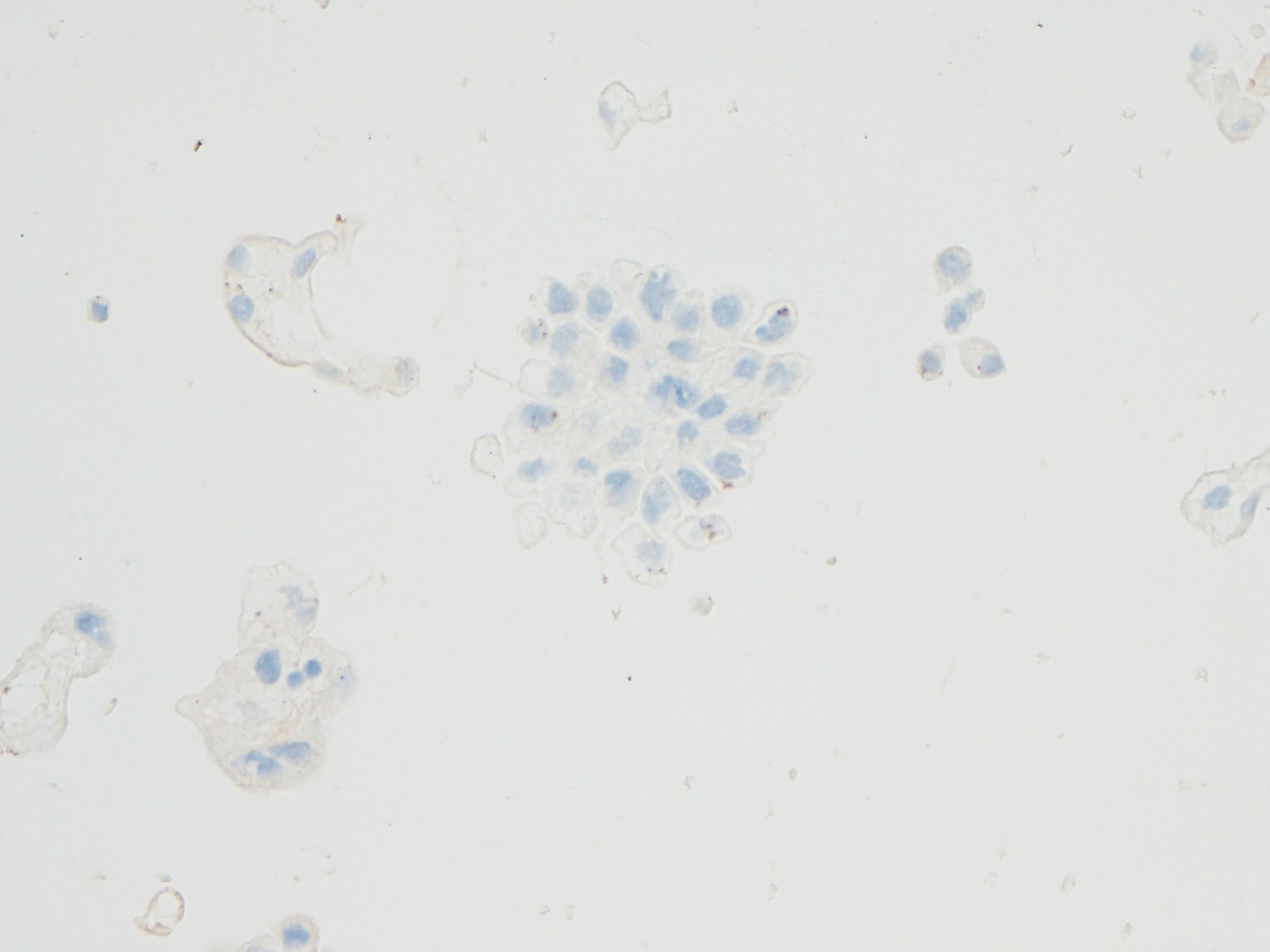 |
|
| Figure 7: PAX8 40x | Figure 8: Calretinin 40x | |
 |
 |
Diagnosis
Patient’s symptoms, imaging studies, cytology evaluation and immunohistochemical profile suggest primary peritoneal carcinoma.
Primary peritoneal carcinoma (PPC) is a relatively rare cancer most commonly found in women. PPC spreads widely inside the peritoneal cavity and mostly involves the omentum and they are often diagnosed in advanced stages. Histologically, it is indistinguishable from serous ovarian carcinoma; however, it spares or only minimally involves the ovaries. PPC is diagnosed in the absence of other identifiable primary sites.
There are different theories to explain the development of primary peritoneal carcinoma. Some authors argue PPC developed from coelomic epithelium lining the abdominal cavity and the ovaries undergoing metaplasia in response to an oncogenic stimulus. Other authors believe ovarian and primary peritoneal carcinomas are of mullerian origin. In fact, the similar clinical characteristics of these tumors suggest that they could be regarded as a single disease entity.
Differential Diagnosis
Malignant mesothelioma
Derived from the peritoneal mesothelium, often associated with asbestos exposure and abdominal radiation exposure. In mesothelioma, the cells grow in multiple layers, form papillary or tubular structures. Histologically, malignant mesothelioma is classified into epithelial, sarcomatoid, and mixed. Calretinin stain would be positive for this case.
Serous ovarian carcinoma
Classified as high grade or low grade. Low grade often have papillary structures with many psammoma bodies, cribriform glands, cysts, or irregular nests of cells. High grade present with branching papillary fronds, slit-like fenestrations, glandular complexity, moderate to marked nuclear atypia with marked pleomorphism, prominent nucleoli, frequent mitoses, and stromal invasion. High grade serous ovarian carcinoma is often associated with P53 mutation.
Tumors express PAX8
- Thyroid carcinoma
Clinical history is important for diagnosis since metastatic tumors can simulate a thyroid primary. For example, at low power the architecture may reveal a papillary or follicular pattern. In addition, classic papillary cytological features may be present which include pseudoinclusions (cytoplasmic invaginations into nucleus), nuclear grooves, and ground glass nuclei. Additional immunoglobulin markers such as thyroglobulin can be helpful to make the final diagnosis. - Renal cell carcinoma
Radiological findings and patient’s clinical symptoms are always helpful in aiding diagnosis. Cytological evaluation often reveals neoplastic cells with abundant vacuolated cytoplasm (from lipid/glycogen), distinct but delicate cell boundaries, and large nuclei with prominent nucleoli. Additional immunohistochemistry markers such as RCC can support the diagnosis.
References
- Roh SY, Hong SH, Ko YH, et al. "Clinical characteristics of primary peritoneal carcinoma". Cancer Res Treat. 39:65–68. 2007.
- Dubeau, L. "The cell of origin of ovarian epithelial tumors". The Lancet. Oncol. 9.12:1191–1197. 2008.
- Altaras MM, Aviram R, Cohen I, et al. "Primary peritoneal papillary serous adenocarcinoma: clinical and management aspects". Gynecol Oncol. 40:230–236, 1991.
- Barda G, Menczer J, Chetrit A, et al. "Comparison between primary peritoneal and epithelial ovarian carcinoma: a population-based study". Am J Obstet Gynecol. 190:1039–1045. 2004.

 Meet our Residency Program Director
Meet our Residency Program Director