Residency Program - Case of the Month
March 2014 - Presented by Rebecca Sonu, M.D.
Answer:
Synovial sarcoma, monophasic type
Microscopic Description:
Synovial sarcoma is a mesenchymal spindle cell tumor which displays variable epithelial differentiation [1]. Although the name implies, the tumor does not arise from or differentiate from synovium. Synovial sarcoma accounts for 5 to 10% of soft tissue sarcomas and can occur from birth to 89 years old. Most cases occur in young adults and in males. Ninety percent of cases occur before the age of 50.
Synovial sarcoma can occur anywhere in the body and is seen most commonly within the deep soft tissues of the extremities, especially around the knees. The tumor frequently arises adjacent to the joints and tendon sheaths [1]. The neck is involved in ~5% of cases and the thyroid gland [2], stomach [3], mediastinum [4], pericardium [5], lung [6], cerebellum [7] and even intravascular sites [1] have been reported in the literature.
Clinically, synovial sarcoma presents with a mass either with or without pain. The tumor tends to grow slowly. Local symptoms depend on the site and size of the tumor. Grossly, the tumor is well circumscribed when slowly growing and infiltrative when advanced. The tumor is usually soft and tan to gray (see Figure 3). Necrosis is seen in poorly differentiated cases.
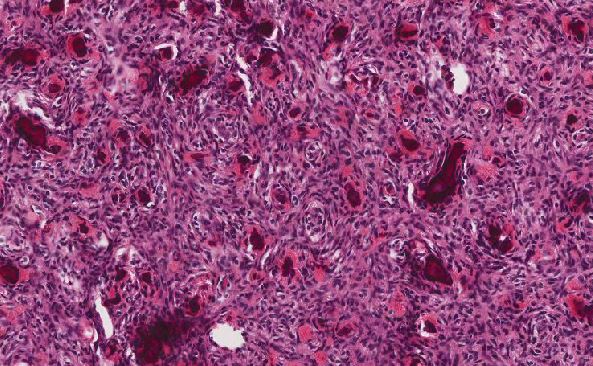
Microscopically, synovial sarcoma can be either monophasic or biphasic. The biphasic type has both epithelial and spindle cell components in varying proportions. The epithelial component can form glands with lumens or papillary structures. Solid cords, nests and squamous metaplasia can be seen [1]. The spindle cell component consists of uniform spindled cells with small nuclei and sparse cytoplasm. The monophasic type of synovial sarcoma often comprises of only the spindle cell component. Architecturally, the spindled cells may display dense cellular sheets or whorl-like fascicles. Myxoid change can be present and mitotic figures are usually rare. About one-third of cases show calcification either with or without ossification.
A third subtype, poorly-differentiated, consists of primitive round cells or larger anaplastic cells with an elevated mitotic activity and necrosis [8].
Immunohistochemical profile of synovial sarcoma [1]:
- Epithelial component = cytokeratin + (90%) [Rare positive in spindle cells]
- EMA+ is expressed more often and more diffusely than cytokeratin
- Spindled cells = diffusely BCL2 + and vimentin +
- Epithelial cytoplasm and membrane of spindle cells = CD99 + (62%)
- CD34 negative
- Desmin negative but focal + for muscle specific or smooth muscle actin
More than 90% of cases of synovial sarcoma will exhibit a specific reciprocal translocation t(X;18)(p11;q11). The translocation leads to the fusion of the SS18 (SYT) gene to one of three SSX genes (SSX1, SSX2 or SSX4). The resulting chimeric SS18-SSX protein is suggested to act as an oncogenic transcriptional regulator [9]. Three types of SS18/SSX fusion products have been seen in synovial sarcomas: SS18/SSX1 (most cases), SS18/SSX2 and SS18/SSX4 [1]. SS18-SSX-induced Wnt/β-catenin signaling appears to be of crucial biological importance in synovial sarcoma tumorigenesis and progression, representing a potential molecular target for the development of novel therapeutic strategies [9].
The differential diagnosis of synovial sarcoma should include:
- Malignant peripheral nerve sheath tumor can show similar histologic and immunophenotypic features especially with the monophasic subtype of synovial sarcoma. The t(X;18) has also been reported in MPNST [10]. MPNST, in comparison to synovial sarcoma, is usually associated with Neurofibromatosis -1. Kang et al, recently showed that SOX-10 is a specific (93%), albeit not very sensitive (67%), diagnostic marker to support a diagnosis of malignant peripheral nerve sheath tumor over synovial sarcoma [8].
- Others: fibrosarcoma, schwannoma, metastatic adenocarcinoma (if mainly epithelial component)
Wide surgical excision is the intervention of choice with post-operative radiotherapy to control local recurrence. Negative surgical margins are important in order to prevent recurrence. In adults, up to 50% of synovial sarcoma recur within a couple of years. Forty percent metastasize most commonly to the lungs, regional lymph nodes and to the bone. The five-year survival is 36-76% [1]. In patients under 20 years of age, inadequate primary excision, tumor site, size, and histological grade should be considered when determining a risk-adapted treatment for synovial sarcoma. Local recurrence and late metastases appear to occur sooner in pediatric patients versus in adults [11]. In patients younger than 20 years old, the overall, 5- and 10-year survival rates were 77 and 61%, respectively [11].
References:
1. Fletcher C, et al. Synovial sarcoma. World Health Organization Classification of Tumors: Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press, Lyon, 2002.
2. Boudin L, et al. Primary synovial sarcoma of the thyroid gland: Case report and review of the literature. Case Rep Oncol. 2014 Jan-Apr; 7(1):6-13.
3. Michot N, et al. Gastric synovial sarcoma: Case report and systematic review of literature. J Gastrointest Cancer. 2014 Mar. [Epub ahead of print]
4. Salah S and Salem A. Primary synovial sarcomas of the mediastinum: A systematic review and pooled analysis of the published literature. ISRN Oncol. 2014 Jan.
5. Yoshino M, et al. Pericardial synovial sarcoma: A case report and review of the literature. Surg Today. 2013. [Epub ahead of print]
6. Kalpathi K, et al. Primary pleuropulmonary synovial sarcoma: A report of two cases and review of literature. South Asian J Cancer. 2013 Oct-Dec;2(4):231.
7. Xiao GY, et al. Synovial sarcoma in cerebellum: a case report and literature review. Brain Tumor Pathol. 2014 Jan;31(1):68-75.
8. Kang Y, et al. Diagnostic utility of SOX10 to distinguish malignant peripheral nerve sheath tumor from synovial sarcoma including intraneural synovial sarcoma. Mod pathol. 2014 Jan;27(1):55-61.
9. Trautmann M, et al. SS18-SSX fusion protein-induced Wnt/B-catenin signaling is a therapeutic target in synovial sarcoma. Oncogene. 2013 Oct 28 [Epub ahead of print]
10. Vang R, et al. Malignant peripheral nerve sheath tumor with t(X;18). Arch Pathol Lab Med. 2000 Jun;124(6):864-7.
11. Speth BM, et al. Synovial sarcoma in patients under 20 years of age: a multicenter study with a minimum follow-up to 10 years. J Child Orthop.2011;5(5):335-342.

 Meet our Residency Program Director
Meet our Residency Program Director