Residency Program - Case of the Month
September 2013 - Presented by Michael Van Ness, M.D.
Answer:
Paratesticular well-differentiated lipoma-like liposarcoma.
Discussion:
Paratesticular malignancies are rare. In adults more than 75% of these lesions arise from the spermatic cord. Most spermatic cord tumors are benign (70 to 80%) and are comprised primarily of lipomas. Liposarcomas are the second most frequent sarcoma in adults and reportedly represent approximately 3 to 7% of all spermatic cord sarcomas.
Spermatic cord liposarcoma usually presents as a painless scrotal swelling that grow in size slowly during a period ranging from months to years. Occasionally a previously stable mass can rapidly increase in size. Average patient age at presentation is 55 years with a slight right side preponderance. Less than 6% of cases have a history of scrotal surgery or trauma. Most authorities believe that liposarcomas arise from mesenchymal cells rather than from malignant transformation of lipomatous cells.
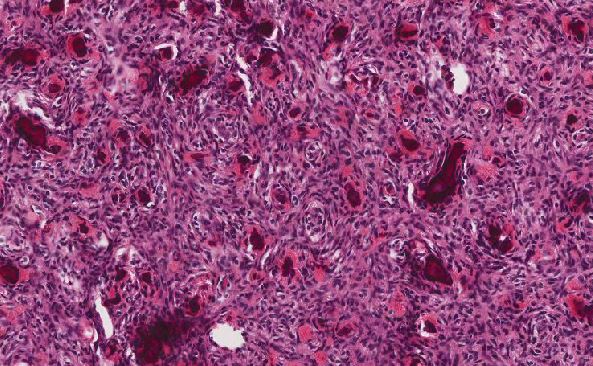
The histological differential diagnosis of well-differentiated lipoma-like liposarcoma consists of other benign fatty tumors, i.e., normal fat or simple lipomas. These can be excluded by the presence of atypical cells with large, hyperchromatic nuclei, either in the fibrous septa or in the fat. These cells can be very focal. Some cases additionally contain lipoblasts, however these are not essential for the diagnosis.
Distinguishing atypical lipomatous tumor-well-differentiated liposarcoma (WDL) from benign adipocytic neoplasms and dedifferentiated liposarcoma (DDL) from pleomorphic or myxoid liposarcoma (LPS) can be difficult. WDL and DDL characteristically harbor ring chromosomes, amplifications of the MDM2 and CDK4 cell cycle oncogenes with protein overexpression, and can also overexpress the cell cycle regulator p16.
The immunohistochemical trio of CDK4, MDM2, and p16 is a useful ancillary diagnostic tool that provides strong support in distinguishing WDLs from other adipocytic neoplasms with a sensitivity and specificity for detecting WDLs or DDLs of 71% and 98%, respectively. Of these three markers, p16 is the most sensitive and specific marker for WDL.
References:
1. Paula J. Woodward, MD, Cornelia M. Schwab, MD, Isabell A. Sesterhenn, MD. From the Archives of the AFIP Extratesticular Scrotal Masses: Radiologic-Pathologic Correlation. RadioGraphics 2003; 23:215–240.
2. Vainrib M. PARATESTICULAR TUMORS. Meir Hospital. www.mednet.co.il/
3. Syed Ali Akbar, MD ● Tawfeeq Amjadali Sayyed, MD ● Syed Zafar Hasan Jafri, MD ● Farnaz Hasteh, MD ● James Simeon Adams Neill, MD. Multimodality Imaging of Paratesticular Neoplasms and Their Rare Mimics. RadioGraphics 2003; 23:1461–1476.
4. Thway K, Flora R, Shah C, Olmos D, Fisher C.Diagnostic utility of p16, CDK4, and MDM2 as an immunohistochemical panel in distinguishing well-differentiated and dedifferentiated liposarcomas from other adipocytic tumors. Am J Surg Pathol. 2012 Mar;36(3):462-9.
5. Amin MB. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Mod Pathol. 2005 Feb;18 Suppl 2:S131-45.
6. B. KHOUBEHI, V. MISHRA, M. ALI, H. MOTIWALA and O. KARIM. Adult paratesticular tumours. BJU International (2002), 90, 707–715.
7. Robert E Emerson, Thomas M Ulbright. Morphological approach to tumours of the testis and paratestis. J Clin Pathol 2007;60:866–880.
8. Matthew J. Horne, MD; Adebowale J. Adeniran, MD. Primary Diffuse Large B-Cell Lymphoma of the Testis. Arch Pathol Lab Med—Vol 135, October 2011.
9. Hiroshi Miyamoto, MD, PhD, Elizabeth A. Montgomery, MD, and Jonathan I. Epstein, MD. Paratesticular Fibrous Pseudotumor: A Morphologic and Immunohistochemical Study of 13 Cases. Am J Surg Pathol Volume 34, Number 4, April 2010.
10. Mahul B Amin. Selected other problematic testicular and paratesticular lesions: rete testis neoplasms and pseudotumors, mesothelial lesions and secondary tumors. Modern Pathology (2005) 18, S131–S145.
11. Robert V Rouse MD. http://surgpathcriteria.stanford.edu/
12. Eugenio O. Gerscovich, Sima Naderi, and Regina F. Gandour-Edwards. Serous Papillary Carcinoma of the Tunica Vaginalis Testis. J Ultrasound Med March 2011; 30:418–422.
13. Thomas C. Winter, MD. There Is a Mass in the ScrotumVWhat Does It Mean? Evaluation of the Scrotal Mass. Ultrasound Quarterly Vol. 25, Number 4, December 2009 195-205.
14. Stephen l. Schwartz, stanley j. Swierzewski, 111, vernon k. Sondak and h. Barton grossman. Liposarcoma of the spermatic cord: report of 6 cases and review of the literature. The journal of urolcgy. Vol. 153, 154-157, January 1995.
15. Montgomery, Elizabeth M.D.; Fisher, Cyril M.D., D.Sc.(Med). Paratesticular Liposarcoma: A Clinicopathologic Study. The American Journal of Surgical Pathology. Issue: Volume 27(1), January 2003, pp 40-47.

 Meet our Residency Program Director
Meet our Residency Program Director