Residency Program - Case of the Month
April 2011 - Presented by Aram Millstein, M.D.
Answer:
Leydig Cell Tumor
Histological description
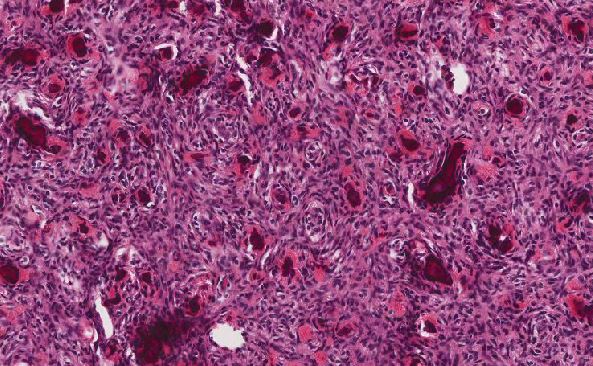
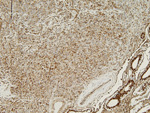
The tumor consists of sheets and cords of tumor cells with an eosinophilic cytoplasm, indistinct cytoplasmic borders, oval nuclei, and prominent nucleoli. Reinke crystals are not identified. Little nuclear atypia is observed, and no mitoses are identified.
Immunohistochemistry
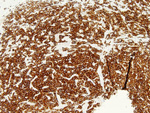
The tumor cells were diffusely positive for inhibin and vimentin.
|
Figure 4. Desmin |
Figure 5. Inhibin |
 |
 |
|
Figure 6. CD30 |
Figure 7. CAM 5.2 |
 |
 |
|
Figure 8. Synaptophysin |
Figure 9. Vimentin |
 |
 |
Discussion:
Leydig cell tumors are the most common type of sex cord-stromal tumors of the testis. They account for 1-3% of testicular tumors. Leydig cell tumors are most common in the third to sixth decade with a smaller peak in children, age 5 to 10 years old. The clinical presentation depends on the age of the patient. Children often present with isosexual pseudoprecocity due to increased androgens from the tumor. They can also develop gynecomastia as the androgens are converted to estrogens peripherally. Adults generally present with a testicular mass. Approximately 30% of adults with a Leydig cell tumor develop gynecomastia. Bilateral Leydig cell tumors are rare.
On imaging, Leydig cell tumors are well defined. They are hypoechoic masses, as in this patient. They may show cystic areas or areas of hemorrhage or necrosis. Their sonographic appearance is indistinguishable from germ cell tumors.
Grossly, Leydig cell tumors are well circumscribed, solid, nodules that are generally 2 to 5 cm in size. Their cut surface is usually yellow to mahogany brown. Foci of hemorrhage and necrosis may be identified in some cases. About 10 to 15% of cases have expansion of the tumor into extratesticular tissue.
On histologic examination the tumor is generally in sheets, although it may also present in nests, ribbons, and cords. Spindled tumor cells arranged in vague fascicles have been described. Usually the cells are polygonal with eosinophilic cytoplasm and distinct cell borders. Abundant lipids can cause their cytoplasm to appear foamy or vacuolated. The nuclei are round to oval with prominent nucleoli. Binucleated or multinucleated cells can be present. Mitotic figures are generally rare. Crystals of Reinke, rod-shaped intracytoplasmic crystals are present in about 40% of cases, although not in this case. More commonly present however, are globular eosinophilic cytoplasmic inclusions that are likely precursors to Reinke crystals.
As in this case, tumors are positive for vimentin and inhibin. Some cases can show cytokeratin positivity.
About 10% of Leydig cell tumors are malignant. Older patients are more likely to have a malignant tumor and tumors that cause gynecomastia are more likely to follow a benign course. Features associated with malignancy include, large size (greater than 5 cm), cytologic atypia, increased mitotic activity (3-5 mitoses/10 hpf), necrosis, and vascular invasion. The tumor in this case was 0.5 cm in greatest dimension, had little atypia, and no increased mitotic activity or vascular invasion; therefore, it is almost certainly benign. Most malignant Leydig cell tumors show DNA aneuploidy and have increased MIB-1 staining. Malignant tumors do not respond to radiation or chemotherapy. Patients with malignant Leydig cell tumors generally develop metastases and have poor survival.
References:
- Mills, SE et al. Sternberg's Diagnositic Surgical Pathology. Fifth Edition, Wolters Kluwer/Lippincott Williams and Wilkins, 2010.
- Kim I, Young RH, Scully RE. Leydig cell tumors of the testis. A clinicopathological analysis of 40 cases and review of the literature. Am J Surg Pathol 1985; 9:177-192.
- Ulbright TM et al. Leydig cell tumors of the testis with unusual features. Adipose differentiation, calcification with ossification, and spindle-shaped tumor cells. Am J Surg Pathol 2002; 26:1424-1433.
- Eble JN, Sauter G, Epstein JI, Sesterhenn IA. WHO: Tumours of the Urinary System and Male Genital Organs. IARC Press, 2004.

 Meet our Residency Program Director
Meet our Residency Program Director