Clinical milestones
Another record-breaking year for Transplant Center

2024 was a record-breaking year for the nationally-recognized UC Davis Health Transplant Center, which gave new life to hundreds of patients in Northern California needing the gift of an organ — often from a stranger.
The kidney transplant program performed 310 kidney transplants in 2024, including 90 from living donors, a UC Davis Health record. The pediatric kidney transplant program set high marks with 12 transplants, also a record.
In the first full calendar year of the liver transplant program, its team performed 44 adult liver transplants — far surpassing its initial year goal of 12 to 14 transplants. The team had a perfect 100% patient survival rate and a graft survival rate of 100%. Both rates are well above the national average of 83%, according to the United Network of Organ Sharing (UNOS).
Hospital leaders said the success results in part from increased communication and collaboration with community partners, such as Sierra Donor Services, as well as international leaders in transplant care who improved patient processes and education.
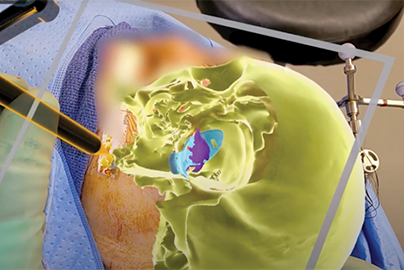
The liver transplant program’s success during its first year can also be attributed in part to the use of a novel technology called liver perfusion. Approved by the FDA, the process circulates fluid and oxygen through a liver that’s already been removed from a donor but not yet transplanted. The process preserves the liver’s function and potentially enhances the recovery process for patients.
“The perfusion process allows the liver to spend much less time on ice without blood flow, which is better for the organ,” said Lea K. Matsuoka, M.D., section chief for liver transplantation and hepatobiliary surgery at the Transplant Center. “Additionally, during the procedure, we are able to better assess the quality and function of the liver before it is transplanted — improving the likelihood of a successful transplant.”
The UC Davis Transplant Center has been a leader in organ transplantation since its inception in 1985. The program serves patients in the 33 counties UC Davis Health covers, which includes a 65,000-square-mile area north to the Oregon border and east to Nevada. It is the only organ transplant program in California north of San Francisco.
“These accomplishments are a testament to our dedicated team members who have helped us develop innovative ways to help patients achieve a transplant,” said Sophoclis Pantelis Alexopoulos, M.D., medical director for the Transplant Center.
UC Davis Health researchers also continue investigating ways to expand the supply of donor kidneys, such as recent studies about optimizing organ assessment and preservation in ex vivo normothermic perfusion and the safety of transplanting from toxoplasma antibody positive donors (TPDs).