The MUSE microscope:
Fast-tracking pathology
For patients who may face a cancer diagnosis, waits can be agonizing.
Biopsied tissue is routed to pathology, where it is sliced, stained and scrutinized. At best, the results will come back the next day. Depending on where the lab is, the process can take a week or longer.
“More than 80 percent of the time, patient biopsies will come back normal,” says Richard Levenson, professor and vice chair for strategic technologies in the UC Davis Department of Pathology and Laboratory Medicine. “Meanwhile, the patient is waiting for results for a potentially lethal disease. They live with a great deal of anxiety.”
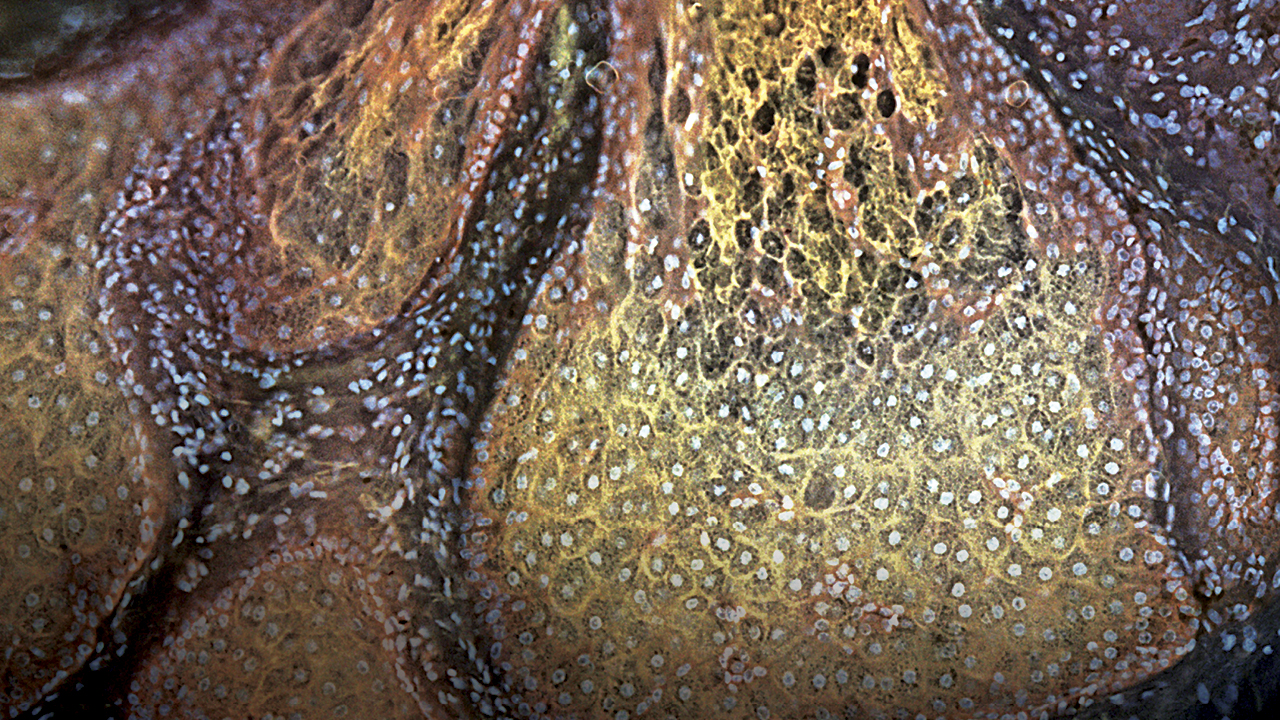
To remedy this, researchers at UC Davis are working on a new way to view tissue. They’ve created the MUSE microscope, which uses ultraviolet rather than visible light. MUSE samples do not require the rigorous preparation that can slow down analysis of conventional slides. This new workflow could speed diagnosis and treatment, making cancer patients’ lives a little better. The researchers recently introduced the technology and its many potential uses in an article in the journal Nature Biomedical Engineering.
MUSE (microscopy with ultraviolet sectioning excitation) started in the laboratory of Stavros Demos, now at the University of Rochester. Demos was using a tunable laser to examine intact tissue. By adjusting wavelengths, he could change what he saw.
Pay dirt came around 280 nm (far below the visible range). Light at this wavelength penetrates tissue only about 10 microns, not much more than the thickness of a microscope slide but without having to actually make the slide. With this new approach, pathologists could examine tissue without the laborious prep.
“It takes a tremendous amount of effort, labor and reagents to make a slide,” says Levenson. “You have to physically cut the tissue. MUSE gets rid of that logistical problem by going straight from tissue to diagnosis.”
While the diagnostic advantages are obvious, MUSE could offer other benefits. Surgical oncologists often send samples to the lab mid-procedure to make sure they get the entire tumor. A fast technique like MUSE could mean less time on the operating table.
Interventional radiologists conducting core needle biopsies could get tissue assessed rapidly to ensure the sample is actually tumor and not healthy tissue or dead cells. Currently, if they don’t get what they need, the patient may need to return for a repeat procedure.
John McPherson, deputy cancer center director and professor in the Department of Biochemistry and Molecular Medicine, is excited because less prep could mean better samples.
“I look at the DNA and RNA from tumors,” says McPherson. “The standard processing is formalin fixation, and the formalin really damages DNA. We’re moving into a precision medicine world, using this genetic material to help make a diagnosis. It would be nice if it were in a little better shape.”
Clinicians like the technology, but first MUSE must be used in clinical trials to prove it’s at least as effective as current methods.
“We have to show that it gives the equivalent diagnosis,” says McPherson. “We’re going to do side-by-side tests, a bake-off, if you like. Once we get preliminary data, we can move on to larger trials.”