Two examples of the kind of research areas being pursued by scientists at UC Davis Health’s new Institute for Psychedelics and Neurotherapeutics.
1. Screening hundreds of compounds to find new addiction treatments related to psychedelics
Evidence from human and animal testing suggests the brain-altering effects of psychedelics could be repurposed for treating addiction.
Now, researchers at UC Davis and the University of Colorado Anschutz Medical Campus plan to screen hundreds of compounds to discover new, non-hallucinogenic treatments for substance use disorders. The research is funded by a $2.7 million grant from the National Institute on Drug Abuse, part of the National Institutes of Health.
 Previous work has shown psychedelic drugs can rewire parts of the brain involved in depression, substance abuse and post-traumatic stress disorder.
Previous work has shown psychedelic drugs can rewire parts of the brain involved in depression, substance abuse and post-traumatic stress disorder.
David E. Olson, Ph.D., associate professor in the departments of Chemistry, and Biochemistry and Molecular Medicine at UC Davis, is searching for similar effects among compounds without the hallucinogenic effects of drugs like LSD. He calls these compounds psychoplastogens, for their ability to modify the brain.
“I’m very excited that NIDA is recognizing the potential that psychoplastogens might have for patients with substance use disorders,” Olson said. “This grant will help us to understand the basic mechanisms by which these compounds impact addiction, and hopefully develop more effective and better tolerated treatments.”
Olson’s work is part of a growing focus on psychedelics research at UC Davis and UC Davis Health. His lab has synthesized hundreds of molecules related to psychedelics in the search for new drug therapies. One such molecule, tabernanthalog, or TBG, produces both rapid and sustained anti-addictive effects in rodent models of heroin and alcohol self-administration.
The research will include mechanistic studies to understand how TBG impacts addiction and the development of new compounds with psychoplastogenic effects, he said. The team will use high-throughput screening to test for efficacy, safety and treatment potential. Promising compounds will undergo additional animal testing at CU Anschutz.
Delix Therapeutics, a startup founded by Olson, is also investigating non-hallucinogenic psychoplastogens for treating depression, anxiety and related disorders but is not involved in the project.
2. Receptor location matters for psychedelic drug effects
Location, location, location is the key for psychedelic drugs that could treat mental illness by rapidly rebuilding connections between nerve cells.
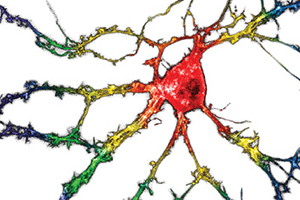
In a paper published Feb. 17 in Science, UC Davis researchers show that engaging serotonin 2A receptors inside neurons promotes growth of new connections, but engaging the same receptor on the surface of nerve cells does not.
The findings will help guide efforts to discover new drugs for depression, PTSD and other disorders, said senior author David E. Olson, Ph.D., associate professor of chemistry, biochemistry and molecular medicine and director of the Institute for Psychedelics and Neurotherapeutics at UC Davis.
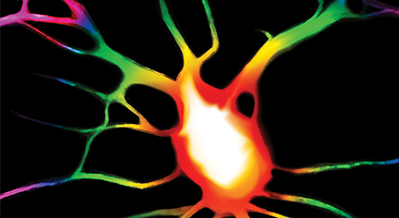
Drugs such as LSD, MDMA and psilocybin show great promise for treating a wide range of mental disorders that are characterized by a loss of neural connections. In laboratory studies, a single dose of these drugs can cause rapid growth of new dendrites — branches — from nerve cells, and formation of new spines on those dendrites.
Olson calls this group of drugs “psychoplastogens” because of their ability to regrow and remodel connections in the brain.
What allows brain connections to regrow?
Earlier work from Olson’s and other labs showed that psychedelic drugs work by engaging the serotonin 2A receptor (5-HT2AR). But other drugs that engage the same receptor, including serotonin, do not have the same growth effects.
 Maxemiliano Vargas, a graduate student in Olson’s lab, Olson and colleagues experimented with chemically tweaking drugs and using transporters to make it easier or harder for compounds to slip across cell membranes. Serotonin itself is polar, meaning it dissolves well in water but does not easily cross the lipid membranes that surround cells. The psychedelics, on the other hand, are much less polar and can easily enter the interior of a cell.
Maxemiliano Vargas, a graduate student in Olson’s lab, Olson and colleagues experimented with chemically tweaking drugs and using transporters to make it easier or harder for compounds to slip across cell membranes. Serotonin itself is polar, meaning it dissolves well in water but does not easily cross the lipid membranes that surround cells. The psychedelics, on the other hand, are much less polar and can easily enter the interior of a cell.
They found that the growth-promoting ability of compounds was correlated with the ability to cross cell membranes.
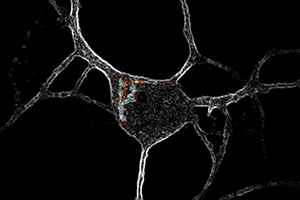
Drug receptors are usually thought of as being on the cell membrane, facing out. But the researchers found that in nerve cells, serotonin 2A receptors were concentrated inside cells, mostly around a structure called the Golgi body, with some receptors on the cell surface. Other types of signaling receptors in the same class were on the surface.
The results show that there is a location bias in how these drugs work, Olson said. Engaging the serotonin 2A receptor when it is inside a cell produces a different effect from triggering it when it is on the outside.
“It gives us deeper mechanistic insight into how the receptor promotes plasticity, and allows us to design better drugs,” Olson said.
Additional authors include: from UC Davis, Lee Dunlap, Chunying Dong, Samuel Carter, Robert Tombari, Lin Tian, John Gray, Shekib Jami, Seona Patel, Lindsay Cameron and Hannah Saeger; Joseph Hennessey and John McCorvy from the Medical College of Wisconsin, Milwaukee. The work was supported by grants from the National Institutes of Health and the Camille and Henry Dreyfus Foundation, and by a sponsored research agreement with Delix Therapeutics.